Class of 2023 Curriculum
Innovating Medical Education
The TCU and UNTHSC School of Medicine brings together the world’s best practices in medical education and the latest advances in technology to forge new boundaries in medical student education and training.
This progressive approach to medical education has been designed to create and shape empathetic scholars who are both adept at caring for patients and able to meet the health care challenges of tomorrow. The student is central to the educational program. Student success is at the heart of the school’s design and has been incorporated in everything from the creation of significant learning experiences and education spaces to the launch of a highly individualized team-based framework for ongoing student coaching and support. The curriculum is divided into three phases across four years and has been carefully crafted to promote learning and student success.
Phase 1 implements an integrated approach to providing students with a foundation in basic and clinical sciences in order to understand the underpinnings of medicine and prepare students to succeed in clinical training.
Phase 2 consists primarily of clinical learning opportunities in a longitudinal integrated clerkship model that will guide students to become proficient clinicians and effective members of a health care team.
Phase 3 is student-focused and allows students the opportunity to pursue a team project in an area of interest as well as to explore career options and fine-tune clinical skills in critical care and sub-internship electives and a number of student-selected electives.
Students can expect a highly-integrated, comprehensive curriculum with content in communication, critical thinking and design, and health care delivery systems among many others, to prepare them for the realities of physician practice in the 21stcentury. The school aims to optimize each student’s experience and performance by using proven strategies in self-directed learning, harnessing new technologies and incorporating longitudinal clinical learning opportunities. Patient care opportunities begin at the time students enter the program and are integrated across the curriculum to provide immersive clinical training experiences and the opportunity for students to develop meaningful relationships with patients and faculty over time. With 24 identified educational program objectives across 7 domains, students can be sure they are receiving the highest quality preparation to excel in the art and science of medicine.
Important Dates + Class Profile
Requirements for M.D. Degree
The school of medicine has required standards for the graduation of medical students. All students who have successfully completed the requirements for the MD degree will be recommended for graduation by the Student Progression and Promotion Committee. For more information, view the Graduation Policy.
Credit Hours
The School of Medicine (SOM) does not use the credit hour as a measure for which students receive credit. However, the weeks of instruction may be converted to credit hours using the following methodology.
The Liaison Committee on Medical Education (LCME), a specialized national accrediting body for all allopathic medical schools, accredits the SOM Integrated Medical Curriculum (IMC). The LCME requires a minimum of 130 weeks of instruction for the MD degree. The TCU and UNTHSC SOM curriculum is 180 weeks over 4 years.
The Southern Association of Colleges and Schools Commission on Colleges is the recognized regional accrediting body in the 11 U.S. Southern states (Alabama, Florida, Georgia, Kentucky, Louisiana, Mississippi, North Carolina, South Carolina, Tennessee, Texas and Virginia) and in Latin America for those institutions of higher education that award associate, baccalaureate, master’s or doctoral degrees.
The SACSCOC requires at least 30 semester credit hours for a doctorate. The TCU and UNTHSC SOM has 180 over 4 years.
For more information, view the Credit Hour Policy.
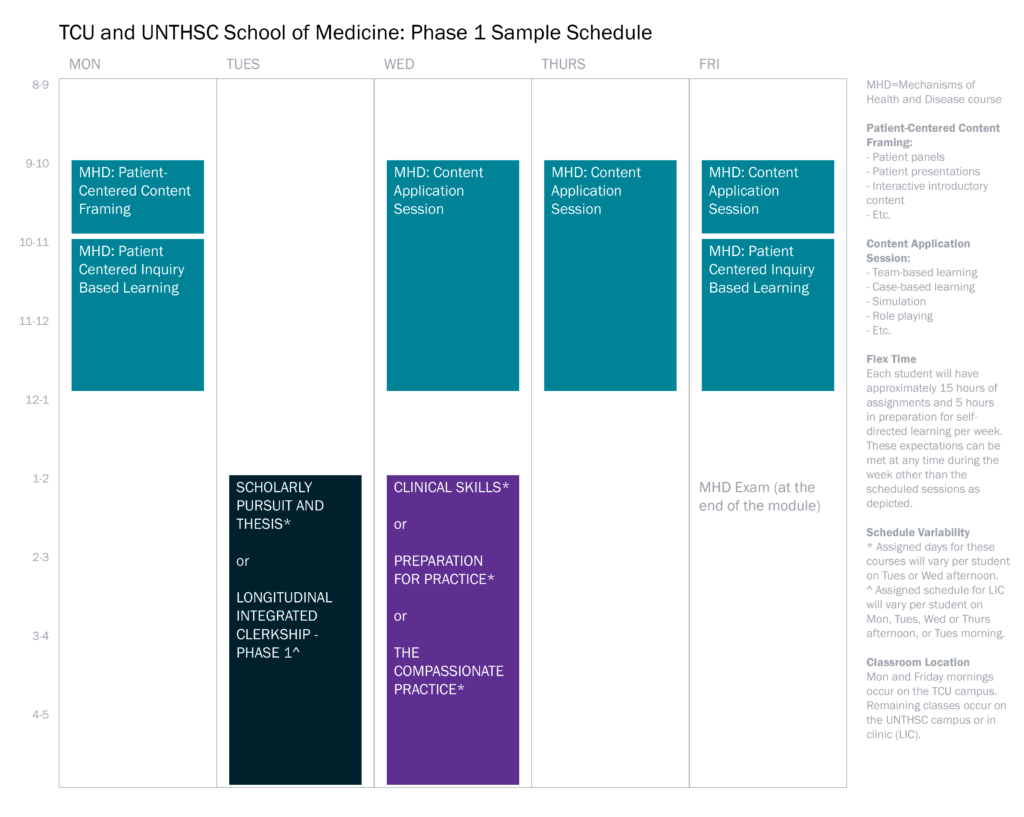
Our student-centered approach limits structured classroom time to less than 20 hours a week. Students have the flexibility to structure 20 additional hours a week for both self-directed and independent study.
A Pass/Fail grading system in Phase 1 encourages a collaborative learning environment. At the beginning of Phase 1, students get an introduction to the requirements and rigors of medical school and clinical practice in the Medical School and Clinical Immersion Course. This provides students a low-stakes opportunity to acclimate to expectations and learn success techniques before embarking on the medical education journey. An organ-based approach will be used to teach basic, clinical and behavioral sciences primarily using structured small group learning in the Foundations; Behavior; Hematology Immunology and Skin; Homeostasis; Neuromusculoskeletal and Metabolism; and Life Cycle courses. Content will also be integrated with other courses throughout Phase 1.
Simultaneously, the students will be able to learn crucial communication and tactile skills, along with clinical reasoning, that that they are able to practice on a regular basis both with standardized and clinical patients, through the Clinical Skills and Phase 1 LIC courses.
They will also begin to explore and develop the skills to become leaders who are able to solve larger problems of practice in health care by utilizing the various techniques from a self-directed learning approach, engaging with the high-tech simulation and technology and beginning to appreciate their role on interprofesional teams, through the Preparation for Practice course.
Students will gain the skills necessary to make evidence-based decisions in clinical practice based upon well-honed research skills taught in the Scholarly Pursuit and Thesis course. Students will also chose their mentor and write a prospectus about a select research project, which they will complete over the four years of the curriculum.
Continuity of patients and faculty in the clinical setting is a cornerstone of our program and begins immediately upon matriculation when students are paired with faculty and a panel of patients with whom they will develop long-term therapeutic relationships that span the all three phases of the educational program. The longitudinal nature of clinical training mimics real-world doctor-patient relationships and allows students to appreciate the continuity of patient care, transitions within the healthcare system and disease progression across time. For the student, being an integral part of a clinical practice and caring for patients over time will foster a meaningful connection and contribution to patient care as well as to the practice environment.
The focus of patient care in Phase 1 is communication, patient education and advocacy. The ongoing, longitudinal engagement with faculty shapes the student’s skills as a clinician as well as their professional identity. There are also substantial opportunities to customize the learning experience including early elective opportunities in Phase 1 where in the Explore and Discover period the possibilities for engagement are endless.
Importantly, the School of Medicine provides a network of individuals who offer personalized academic and professional coaching to students in order to ensure success. Students have access to dedicated Academic Coaches and Executive Coaches who provide support and coaching during this critical time of adjustment and development in a medical student’s professional formation.
Phase 1 Course Descriptions
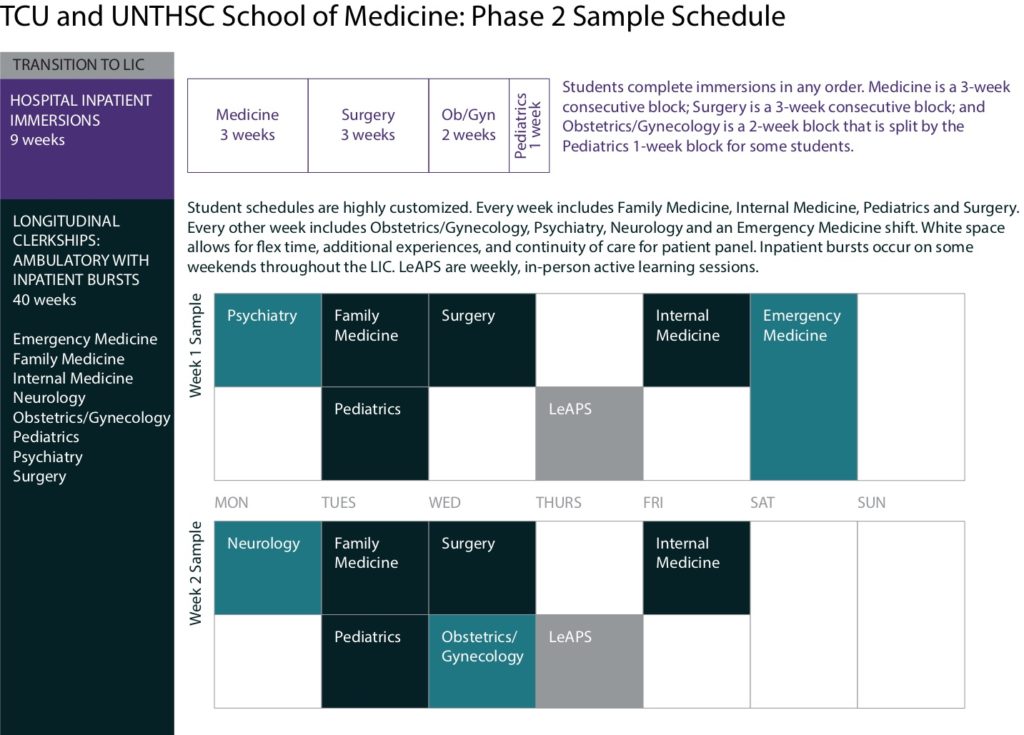
Students will have the opportunity to be an integral part of the health care team in both inpatient and outpatient settings as part of the hallmark Longitudinal Integrated Clerkship (LIC). While most of the clerkship year will occur in outpatient settings, meaningful inpatient experiences are essential. Inpatient immersion experiences at the beginning of Phase 2 will orient students to the hospital environment and their role on the care team as well as help them learn to care for acutely ill patients. Students experience inpatient immersions in the Internal Medicine, Obstetrics and Gynecology, Pediatrics and Surgery clerkships. Additionally, students will complete other shorter inpatient immersion experiences at various intervals for each clerkship, work multiple emergency medicine shifts, and work a weekend of inpatient call per month to expose them to inpatient medicine and the acute conditions that their patients will face. Anesthesiology, pathology, and radiology will be integrated into the experiences at various times during the year. Additional learning experiences have also been designed for Family Medicine, Psychiatry, Neurology and Emergency Medicine clerkships that include exposure and management of both acute and chronic illness in unique settings.
The advantages of longitudinal clinical training are many. The LIC model is both patient-centric and learner-centric; it is a progressive curriculum that enables students to maintain continuity with patients and expand their ability to understand and manage the contemporary complexities of patient care. Clinical teachers are essential members of the educational team and key role models for students. Our clinical faculty have excellent professional reputations; the highest skill and regard for quality and patient-centered care; and a contagious spirit of learning.
For the student, being an integral part of the health care team will foster meaningful learning about patient care and the health care system from faculty who become student advocates over time. Additionally, the LIC schedule allows for ample independent study time for students and opportunities to connect with faculty in small-group learning sessions, called Learning and Pondering Sessions (LeAPS) to focus on connections between the basic and clinical in a supportive team-based learning environment. The final portion of this phase will include time to study for and take USMLE Step 1.
Phase 2 Course Descriptions
Phase 3 begins in the third year and continues until graduation. Students will continue their professional development and scholarly pursuit as well prepare for residency. Students then begin the “Develop” portion of Phase 3 where there is a thematic emphasis on 10 content areas the school has designated as critical to a well-rounded physician practicing 21st century medicine. Groups of students will work with faculty and Physician Development Coaches to develop a focused project related to one of seven societal issues. Students will also continue to care for a small subset of their patient panel, including those they acquired during Phase 1, in order to maintain clinical acuity and allow for a continued connection with patients and clinical teachers. Finally, the students will also have dedicated time to not only continue work on their 4 year project in the Scholarly Pursuit and Thesis course, but will begin to present data to each other in small groups to hone communication skills and collaborative thinking about research.
The next portion of Phase 3 is the “Focus” portion, a truly individualized portion of the curriculum that will include a 4-week sub-internship rotation in a specialty of choice, a 4-week critical care selective in a specialty of choice, and 28 weeks of elective course time to allow students to gain valuable clinical experience, explore career interests and prepare for the residency match process. Students will also be given a generous allotment of time to apply and interview for residency admission, as well as prepare for and take USMLE Steps 2 CK and CS. Finally, the students will enter the “Prepare” portion of Phase 3. Students will participate in a 5-week course entitled Preparation for Residency Boot Camp designed to prepare students for the next stage of their career as a first-year resident. The curriculum will include content on advanced clinical procedures, communication skills, leadership, team management, and other requisite skills. Learners will also complete a course entitled “Final Reflections: The Art of Medicine.” The course will allow time for the students to reflect on their progress through medical school, what it means to be a physician and includes a final emphasis on communication, empathy, and the value of compassionate patient care. During this portion of Phase 3, the students will present their Scholarly Pursuit and Thesis project in the annual research symposium.