Place Card
Prisca Mbonu, Class of 2026
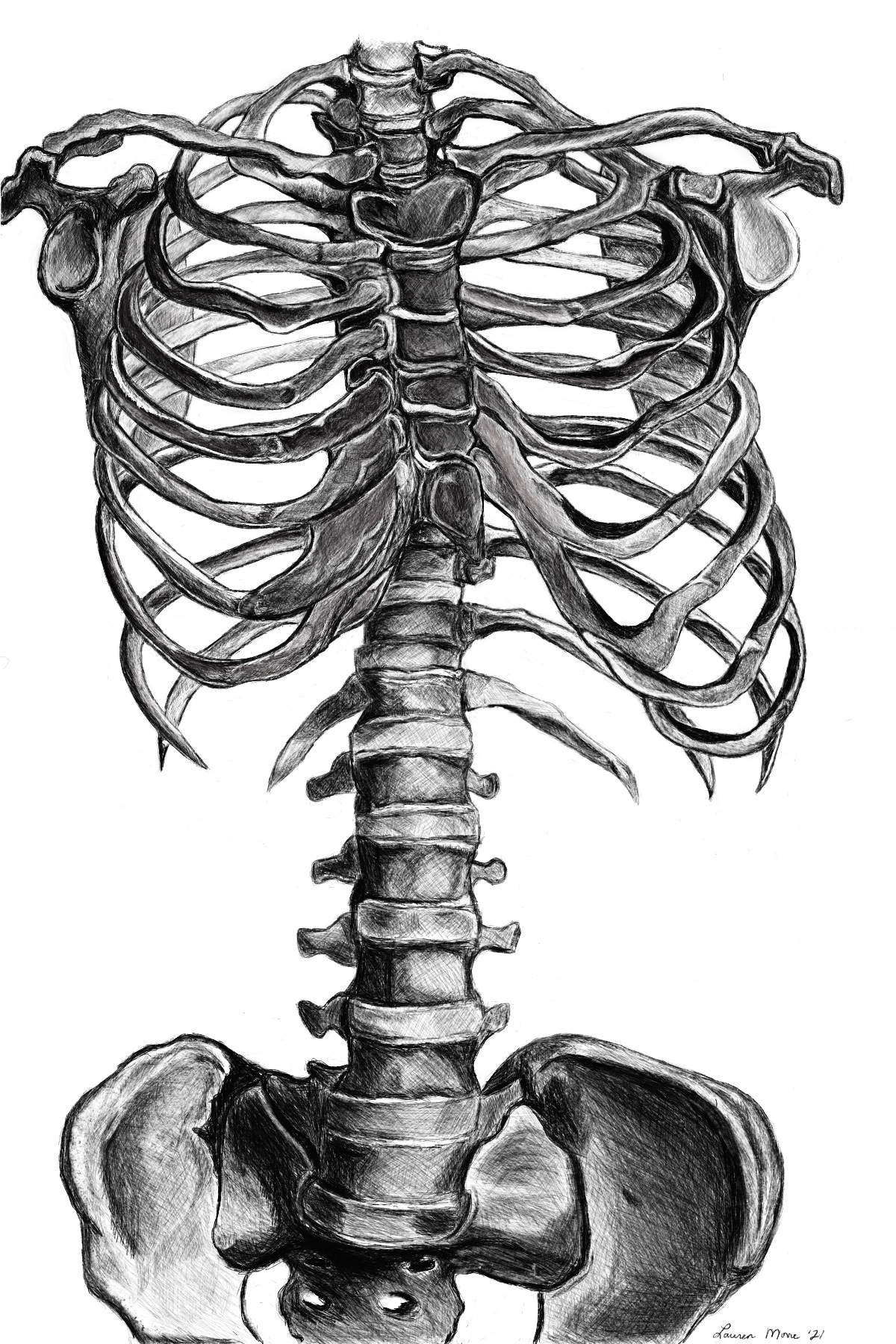
The first step into the Cold cadaveric laboratory The first whiff of formaldehyde That seems to permeate the walls The first moment when the shiny...
Read MoreWelcome to HuMed, a hub to engage in innovative, multidisciplinary practices in medical humanities. Along with faculty-led workshops, HuMed will welcome guest artists from around the country to share their knowledge and best practices in the field of humanities in medicine. The HuMed journal is a medical humanities and creative non-fiction online publication featuring thematic writing, along with other forms of humanities-based contributions from students, faculty, and staff.
Prisca Mbonu, Class of 2026
The first step into the Cold cadaveric laboratory The first whiff of formaldehyde That seems to permeate the walls The first moment when the shiny...
Read More
Prisca Mbonu, Class of 2026
The first step into the
Cold cadaveric laboratory
The first whiff of formaldehyde
That seems to permeate the walls
The first moment when the shiny zipper is pulled
To reveal what is hidden beneath
The first cut through skin
Into fat, fascia, and finally, muscle
The first surge of guilt
At the sacrifice of another
The first feeling of gratitude
Towards a complete stranger
There lies a place card
Mounted against a rusting metallic stand
With words printed on a purple, laminated sheet
They tell me what is left of you
Age. Sex. Cause of death.
But your body tells an even greater story
Of pain, surgical scars
Of adventures, tattoos
Of joy, laugh lines
Of hard work, calluses
Of life, childbirth
In you, I see a collection of firsts too
Ngoc Bao Nhi “Mariana” Nguyen, Class of 2027
Part A (Brief description of chief complaint): Iron Deficiency Anemia: Iron is essential in making hemoglobin, a protein in red blood cells. Iron deficiency anemia...
Read More
Ngoc Bao Nhi “Mariana” Nguyen, Class of 2027
Part A (Brief description of chief complaint):
Iron Deficiency Anemia: Iron is essential in making hemoglobin, a protein in red blood cells. Iron deficiency anemia is a condition in which blood lacks adequate healthy red blood cells due to low level of iron. Common symptoms include fatigue, irregular heartbeat, pale or yellowish skin, and cold hands.
Part B (Poem):
I lack red blood cells
Lightheaded, sometimes I get
I need grass-fed beef.

Ngoc Bao Nhi “Mariana” Nguyen, Class of 2027
Part A (Brief description of chief complaint): Iron Deficiency Anemia: Iron is essential in making hemoglobin, a protein in red blood cells. Iron deficiency anemia...
Read More
Ngoc Bao Nhi “Mariana” Nguyen, Class of 2027
Part A (Brief description of chief complaint):
Iron Deficiency Anemia: Iron is essential in making hemoglobin, a protein in red blood cells. Iron deficiency anemia is a condition in which blood lacks adequate healthy red blood cells due to low level of iron. Common symptoms include fatigue, irregular heartbeat, pale or yellowish skin, and cold hands.
Part B (Poem):
When the iron is running low,
A shadow of fatigue begins to grow.
Pale echoes in each step I take,
Anemia’s weight, a heavy ache.
In veins, a river without its might,
Transferrin, the captain, lost in the night.
Cells, like soldiers, weary and dried,
Battling fatigue, a crimson tide.
When the iron is running low,
Hematocrit staggers below.
Heart’s rhythm stumbles in faltering beat,
A symphony of exhaustion, a silent defeat.
Blood cells fade in ghostly wail,
In the mirror, my complexion pale.
Cold fingertips where blood don’t flow,
When the iron is running low.
A labored sigh in every breath,
Iron’s death, my own Macbeth.
The world spins, a dizzying show,
When the iron is running low.
Iron returns in distant dreams,
In languor’s grip, a silent scream.
Yet hope lingers like a resilient ember,
For iron’s return, a strength to remember.

Ngoc Bao Nhi “Mariana” Nguyen, Class of 2027
Part A (Brief description of chief complaint): A cold is a common viral infection of the nose and throat. Symptoms include runny nose, sneezing, and...
Read More
Ngoc Bao Nhi “Mariana” Nguyen, Class of 2027
Part A (Brief description of chief complaint):
A cold is a common viral infection of the nose and throat. Symptoms include runny nose, sneezing, and congestion. Because antibiotics only fight bacteria, and not viruses, they’re usually ineffective against colds. The condition is usually harmless and mostly resolves on its own within two weeks.
Part B (Poem):
With sniffles and sneezes, he caught a cold,
In bed he rested, his sinus consoled.
No pills would he take,
Just warm tea with cake,
A viral invasion, not bacteria, behold!
Naimah Sarwar, Class of 2025
And he beams, I’m golden, just golden. I’m golden and also, what exactly is a seizure? You see, he’s been drinking that Golden liquid, his...
Read More
Naimah Sarwar, Class of 2025
And he beams,
I’m golden, just golden.
I’m golden and also,
what exactly is a seizure?
You see, he’s been drinking that
Golden liquid, his golden ticket
home. His ticket back to
his golden days, a golden daze.
That heart of gold irradiating
his skin.
Will you think about quitting?
A crescent moon, ear to ear.
I’m golden,
everything is golden.
Golden boy
his eyes, all that glitter.
Jayesh Sharma, Class of 2027
Part A (Brief description of chief complaint): Migraine with aura is a type of migraine headache characterized by the presence of sensory disturbances, known as...
Read More
Jayesh Sharma, Class of 2027
Part A (Brief description of chief complaint):
Migraine with aura is a type of migraine headache characterized by the presence of sensory disturbances, known as an “aura,” preceding or accompanying the headache. The aura typically involves temporary, reversible visual, sensory, or language disturbances that develop gradually over several minutes and usually last for less than an hour.
Part B (Poem):
My eyes open to stark cacophony
Sharpened colors,
Cutting me with their keen vibrancy
Jagged sounds,
As if hitched breaths
Hiding from nearby pursuit
I blink rapidly
Trying to find my place;
A lone straggler
Moored on a lost island
A cloud passes
Rolling past brief farewells
Frosted pearls
Flooding into a conductor’s crescendo
A neighbor glances
Assuming narcissistic attention
Brief windows opening
Caught under heavy fantasy
A babe wails
Fighting confusion with volume
A solo instrument
Caught between fractured arpeggio
I try to stay afloat
flailing with a fool’s futility
Assuming survival
to be adequate reprieve
These blurred lines adjust
as grief tends to do
Moving from pounding beats
unto dull aches
Dragging marionette limbs
Into rehearsed movement
The moment passes
Or perhaps I tell myself it does
Swaying to faint decrescendo
Distraction replacing reality
An easy pivot,
One I have grown accustomed to
Both eyes close once more
Doorways bleeding light
from what they hide behind;
A hopeful illumination
A slight knocking,
as if not to startle beauty awake
I relish my brief ignorance
Into the dread of inevitable beginning
as if sensing a conductor’s crescendo
Building up into a familiar movement
Slowly,
Towards stark cacophony

Jayesh Sharma, Class of 2027
My father bought a ping pong table. It's nothing special. Two sides of green space separated by a thin, rectangular net. Blue and red-halved paddles,...
Read More
Jayesh Sharma, Class of 2027
My father bought a ping pong table.
It’s nothing special. Two sides of green space separated by a thin, rectangular net. Blue and red-halved paddles, built to accentuate each “tick” and “tock” between opposing sides.
He always asks me when I want to play. It’s as if he wants to justify the hassle of getting this table by using it as much as we can. He was the same about his pizza maker, camera, and lawnmower. He’s a dad in normal ways like that, finding color to tint dull days.
Playing with him is quiet.
“Tick.”
“Tock.”
“Tick.”
“Tock.”
“Ti- ah, close.”
At times, between hits, a conversation will ripple between us. It’ll be something small; maybe mom’s latest gripes, Shruti’s upcoming dance performance, or pieces of wisdom he likes to impart.”
Mostly though, it’s quiet.
“Tick.”
“Tock.”
“Tick.”
“Tock.”
“Ti- ah, I’ll get it.”
It’s a steady beat, one I feel my thoughts playing cadence to. It’s calming, letting me flow as my paddle does.
He spent the first five minutes of our time today adjusting things in our garage. He then felt finicky about how centered the table was, and then about how many balls he could hold. Growing up, these tendencies of his would’ve annoyed me to no end; I would’ve felt that he was wasting time while I just wanted to play. That old feeling hinted upwards still, but now I see things a bit more from his perspective. I realize that he was expressing how he wanted our time together to go smoothly, adjusting small things as his way to protect our time.
I haven’t always liked my dad. I used to feel he was the epitome of who I didn’t want to be. I would then feel frustrated that I still admired him for his intellect and work ethic. We used to argue a lot, especially after my sister was born. Everything, from my independence to his anger, was constantly put on the table with no reprieve. Small times like these, ones where we can quietly enjoy each other’s company across the table, show how far we have come.
“Tick.”
“Tock.”
“Tick.”
“Tock.”
“Tick.”
“To-I have another one, leave it.”
I haven’t always been the best son. But he’s been okay with that. In spaces where our conversations ripple, he’s understood the storm which has come before. We’ve both had irrational times with each other, but we always knew that we would always be in each other’s lives. Sometimes, that fact annoyed me more than anything else.
“Tick.”
“Tock.”
“Tick.”
“To- there we go. Last one?”
“Sure, I’m losing breath anyways.”
Two sides of green space separated by a thin, rectangular net. Blue and red-halved paddles, built to accentuate each “tick” and “tock” between opposing sides. That’s how I used to feel with him. Growing up has allowed me to see that it isn’t that way. At some point, we put down the paddles and walked away together. The ripples calmed, the storm passing.
“Tick.”
“Tock.”
“Tick.”
“Tock.”
“Tick.”
“Tick.”
“Tock.”
“Tick. I technically cheated on the last one.”
“Tock.”
“Tick. Ah well, who’s keeping score anyways.”
“Tock.”
“Tick.”
“Tock.”
…
“Want to play again tomorrow?”
“Sure dad.”

Prisca Mbonu, Class of 2026
We entered the procedure room to find the final patient of the day, Ms. K, sitting upright on the examination table. She had already changed...
Read More
Prisca Mbonu, Class of 2026
We entered the procedure room to find the final patient of the day, Ms. K, sitting upright on the examination table. She had already changed out of her own clothes and into the customary light blue patient gown, with a white sheet draped over her legs. Her manicured hands were clasped together, fingers wringing with uncertainty. “Hello, Ms. K,” my preceptor, Dr. L, greeted. “I have a medical student with me today. Are you comfortable with her observing your procedure?” Ms. K’s gaze shifted towards me, and after a moment of hesitation, she nodded slowly and said, “Sure. The more the merrier, I guess.” After thanking her, I gave my introduction, a routine practiced countless times during my two years of training.
My preceptor handed Ms. K two consent forms which clearly stated the risks and benefits of the procedure. I watched as Ms. K’s barely audible sighs accompanied the turn of each page as she read before eventually signing her consent. Soon after, we were joined by two nurses, bringing the room’s occupancy to a total of five. The procedure we were preparing to perform was an endometrial biopsy. Ms. K, a 58-year-old woman, had been experiencing postmenopausal vaginal bleeding for some time. In such cases, an endometrial biopsy is often an initial test for evaluation.
The procedure involves inserting a device into the uterus to collect samples to help determine the source of bleeding. Understandably, patients often find this procedure to be unpleasant and painful, which contributes to heightened levels of anxiety. Furthermore, the potential outcomes of the procedure only serve to worsen this anxiety. This wasn’t Ms. K’s first experience with the biopsy; she recounted her previous ordeal where inconclusive results left her disheartened and without answers. I understood her frustration at the entire situation, her escalating worry about her troubling symptoms, and her desperate need to finally have a diagnosis.
So did Dr. L, who gently held Ms. K’s hand and assured her that, while some discomfort was inevitable, she would do her best to minimize it. The reassurance brought a grateful, tearful nod from Ms. K, and the room’s atmosphere softened. The rest of us chimed in with words of encouragement, and I noticed Ms. K starting to feel more at ease. “Ok. I’m ready,” Ms. K said with a weak smile. While one nurse assisted Ms. K into the lithotomy position, the other organized the required instruments on a stainless steel tray. As the nurse explained the functions of the speculum, tenaculum forceps, Allis clamp, uterine dilators, and suction curette for my learning, I instinctively positioned myself to block Ms. K’s view of the instruments, fearing that seeing them would amplify her anxiety.
As we prepped, we engaged Ms. K in conversation about her background. We learned that she was born in the Caribbean. She spoke wistfully of the beauty of her homeland, painting vivid pictures of breathtaking beaches adorned with rolling waves and caressed by gentle breezes. She reminisced about cerulean skies and distant horizons that beckoned her each morning. Somehow, the conversation veered into light-hearted banter about handsome men from the islands, eliciting hearty laughter from all of us.
Her nostalgia momentarily distracted her from the impending procedure, but she was brought back to the present at the insertion of the speculum to visualize her cervix. She winced, a soft whimper escaping her lips. “Would you like one of us to hold your hand? You can squeeze tight if it hurts,” Dr. L offered. “Just try not to break our medical student’s arm,” a nurse quipped, and more laughter reverberated through the room with Ms. K joining in. In that room, where tension and camaraderie were intertwined with one patient at the heart of it all, I felt a strange sense of kinship among strangers. Once again in my training, I was reminded of how connections could be found in the most unexpected places.
Throughout the procedure, we continued to offer words of encouragement and lighten the mood with jokes. Ms. K kept her eyes tightly shut, breathing shallowly through pursed lips. Occasionally, a faint smile crossed her strained features. I wondered if behind her closed eyelids, she envisioned scenes of deep blue waters and golden sands from her childhood. When the procedure concluded, I bid farewell to Ms. K and made a mental note to follow up on the biopsy results. I hoped they would provide the answers she needed and bring her the relief she deserves.
Kenneth Le, Class of 2027
Part A (Brief description of chief complaint): Mitral stenosis is the narrowing of the mitral valve leading to reduced blood flow between the left atria...
Read More
Kenneth Le, Class of 2027
Part A (Brief description of chief complaint):
Mitral stenosis is the narrowing of the mitral valve leading to reduced blood flow between the left atria and left ventricle. It can lead to complications such as arrhythmia, heart failure, and thromboembolism.
Part B (Poem):
Rheumatic fever
Fused to my friend, I am stuck
Snap then a rumble

Andrew Armstrong, Class of 2027
Part A (Brief description of chief complaint): Psoriasis is a skin disorder affecting individuals with an underlying genetic predisposition who have been exposed to a...
Read More
Andrew Armstrong, Class of 2027
Part A (Brief description of chief complaint):
Psoriasis is a skin disorder affecting individuals with an underlying genetic predisposition who have been exposed to a “triggering event” such as an infection or medication. Psoriasis manifests as a red, scaly, intensely itchy rash that can occur anywhere, but are especially prevalent on the head, elbows and knees. The rash bleeds easily when picked and can even cause other symptoms like pain in the hands and back, as well as finger and toe nail disfiguration.
Part B (Poem):
I itch my arm, I don’t even realize I do it anymore
It bleeds, it usually does
I don’t realize when that happens anymore
I do realize when people stare, that’s harder to get used to
And they never stop, never
I feel like the lepers of biblical times
They were deemed unclean to live among others
I’m deemed unfit to be ignored
So I pick, I bleed, people gawk
Med students analyze
Tired residents check me off their list of “to-dos”
Attendings use me as a teaching point
But they stare too, they all do
And they never stop, never
I get jealous of the other disorders
Things like burns, broken bones, cancer even
At least people know they can’t get cancer from being around people with it
People always wonder if they can get what I have
Then I feel guilty for that thought
At least this won’t kill me
But I would give the anything for it to stop
Jesus healed the leper
If he came and healed me I wouldn’t forget to say thank you
I wonder if he’d stare too

Ope Duyile, Class of 2026
Polycystic Ovarian Syndrome. Cysts on my ovaries? The shock of it all. Reproduction is not until the next block, I don’t know much…yet PCOS The...
Read More
Ope Duyile, Class of 2026
Polycystic Ovarian Syndrome.
Cysts on my ovaries? The shock of it all.
Reproduction is not until the next block, I don’t know much…yet
PCOS
The PA is talking of metformin and birth control
Isn’t that a diabetic medication? Why would I need it?
I’m too scared to ask. It cannot be. Liiiiike, say it ain’t so.
PCOS
My skin is breaking out.
My neck has gotten darker.
The irregular and painful periods.
The insomnia.
The crazy sweet tooth.
My hair has been thinner lately.
My testosterone is elevated.
The rapid weight gain. The struggle with weight loss. My frustrated efforts.
It all makes sense. It is not entirely my fault. I should not have been so hard on myself.
PCOS
I am a medical student on the other side of a scary diagnosis.
I think about all the ways I want my provider to show up.
I wish I had more time to process and ask my questions.
I wish my message on the patient portal was addressed.
I see medicine from a new angle.
I resolve to be a rock when I deliver an unsettling diagnosis.
To avail myself to my patient through the uncertainty and stages of grief.
PCOS
I scour every article PubMed has to offer. C.R.A.P style.
Something about inositol imbalance and insulin resistance. Metformin begins to make sense.
Something about fertility. I want to be able to have children.
With options come power.
I remember that I am still human. This body of mine is frail. I am angry and disappointed
Why me? I have always had a clean health bill.
When did things change and how did I not notice?
Why didn’t this PA tell me more?
Where do I go from here? What is to come?

Mary Howerton, Class of 2024
Your first climb started so young and performed. From so young you had to climb your way out of terrible memories, hard pasts, tough situations....
Read More
Mary Howerton, Class of 2024
Your first climb started so young and performed. From so young you had to climb your way out of terrible memories, hard pasts, tough situations. Rough childhoods or terrible families, military deployments that showed you the worst humanity can be. That first drink was a surprise, an oasis in a desert of misery. For the first time, you had numbness in your life, and you thought it was the perfect solution. Buddies drinking in barracks or in bars. Drinking culture at its prime, giving you permission to get numb.
Was your next climb the ascent? Noticing you drank more than everyone around you? Starting to drink alone, at home? Perhaps you thought no one would notice. Sneaking away from the family you had to find numbness again. You love them, it’s not them you want to hide from. The drinks you have don’t seem to be enough anymore. Higher count, higher proof, higher concentration to attempt the same high as before. For a time, you couldn’t tell which was the stronger drug- alcohol or denial.
You climbed deeper and deeper into addiction at that point. Physical dependence replaces any psychological one you had previously. Baseline levels just to not feel sick, but those levels made you feel bad anyways. Tremors, sweats. Cutting back but you couldn’t. Feeling stuck. The life you have and the life you want separated by the chasm that is withdrawal.
Climbing into darker and darker depths. And then that news. “We have run some tests and we have important news to share with you. You have cirrhosis or scarring of the liver. Based on your symptoms, your liver is failing to do its job. We will do everything we can to keep you as healthy as we can, but we need to start looking at other options”. In that moment the warm blanket of denial is ripped away. Cold reality sets in. The chill on the path you have set for yourself is so lonely and so cold. Regret is bitter. And there a decision had to be made; do you continue the road you were on, or do you choose an entirely different battle?
The road to sobriety was one of the toughest climbs you have ever had. While I might have some clue about what that entailed, only you know the strength it took to change it all.
Perhaps the most complicated part of this route was what lay ahead. Transplant committee meetings. Transplant lists based on scores. Review boards and waiting for a second chance. All the while your body fights every day to keep up. Fatigue setting in, skin and bones. Yellow and sunken eyes. The body a betrayal of the work you put in the last six months to fight for sobriety.
The days are long, but you keep walking. Your steps slow, and you notice yourself stumbling every few feet. Then falling to your knees. You can’t climb anymore, you think. Collapsing down. You can see the ascent, the end. But it is too far away.
I come visit you in the intensive care unit. Your body is failing, and we have hooked up to every machine we could to keep you alive until a donor is available. Intubated and sedated you lie there, holding onto life. I pull out my notes from my white coat, write down the newest numbers on how you are operating. Notes put away. I grab your hand. I plead and pray for a new liver for you. For a second chance at a mended life. We stay like this for a while before I let you rest for what will be the last ascent, the transplant surgery.
You received your second chance at life at 11:56 pm that same day. Keep climbing. You have already come so far.

Kenneth LeCroy, MD
There is an old joke that asks the question, “How do you want to die?” The answer is a quipping one: “I want to die...
Read More
Kenneth LeCroy, MD
There is an old joke that asks the question, “How do you want to die?” The answer is a quipping one: “I want to die like my grandfather, peacefully in his sleep. Not screaming, yelling, and in terror like all his passengers.” A silly joke asking a very important question.
One of the early steps in Stephen Covey’s book 7 Habits of Highly Successful People is to start with the end in mind. He means to begin by visualizing a life goal and then build foundations and processes that help to accomplish that eventuality. Those goals may or may not be achieved, but the eventuality of death will happen to us all. So how do you want to die?
I would like to tell you a great way to die, but before I get there, I have to tell you some stories.
In 1991 my oldest brother David had a dream that essentially pushed our younger brother and me to go on a five-week trip to and through Alaska. We drove to the Canadian border from San Antonio, Texas—and that was just the halfway mark. (We made it work, but this is not how I recommend traveling North.) Our first stop was Skagway, Alaska to do the fairly grueling Chilkoot trail, a 33-mile stretch of the Yukon Gold Rush. The elevation gain is incredible, with up and down sections repeating ad nauseum. We began the three-day trek with 35-pound packs and were out of food by the last day. On our second day, we were concerned about a group camping nearby—three friends, one in their late 70s, the other two in their 80s. We were discussing whether to share our food with them when we heard the distinctive sound of a bottle of wine opening! We later wondered if we should offer to help them at the pass itself…and they beat us to the top. Had we known we would have been asking them for their help throughout the trip as they were clearly living their best lives while ignoring the number of their birthdays.

We had done the trail. A three-day hike that was a great accomplishment in life. We sat in silence among debris and trash from me that had lived and loved and worked so hard and died one hundred years before us. A humbling moment.
Fast forward 10 days from there. We were in Denali National Park where cars are not allowed. Ingress is by yellow school buses to which the animals have acclimated. We had plans to camp for 7 days, so we packed heavy 55-pound packs and rode the bus for five hours before embarking on a flat 7-mile hike to our site.
The moment we strapped on the packs it was vastly different— I still use this illustration with patients about the benefits of losing 20 pounds. We trudged our way through thick high brush, calling out every 20 or 30 seconds “Hey Bear!”; walking up and surprising an Alaskan grizzly is not wise. After a rest break on the first day, we all struggled like crazy to get on our feet again. David in particular struggled, he slipped and found himself on his back with the backpack weighing him down, as helpless as an overturned turtle. Far from being angry, David laughed uproariously, and the three of us laughed continuously for a long time. From time to time over the years, we talk about that trip to Alaska and always include that moment.
Fast forward now to the Christmas of 1998. My family as a rule would gather for at least a weekend around Christmas to celebrate, and this Christmas was no different. I clearly remember my brother David asking me a question that puzzled me at the time. He asked, “You know that feeling you get when you pass out while you’re laughing really hard?“ I told him that I did not know what he was talking about, and I left it at that. A month and a half later on Valentine’s Day, there was another family gathering to celebrate my mother’s and my brother David’s birthdays (his 35th.) I was unable to go but my wife made it. She mentioned that David was experiencing balance issues and she had seen him hit a wall once while walking down a hallway. He assured everyone that he had seen his doctor and had an MRI pending. A few days after returning from that Valentine’s visit he had the MRI results—and an appointment his primary care doctor had scheduled with an oncologist. I was able to go with him to that oncology appointment. I was completely convinced that he had an acoustic neuroma—difficult to treat, but treatable.
David and I went into the appointment room together. It was a small exam room in the Cancer Treatment and Research Center of the University of Texas Health Science Center at San Antonio. Along one wall was a bank of X-ray view boxes and MRIs attached to the wall. Instantly I was disappointed in the center because they had clearly left the previous patients’ MRI up and allowed David and me to enter. I briefly glanced at the X-rays and could see an obvious large tumor…the previous patient was, as our Alabama relatives would say, an absolute dead person. I was approaching the end of my third year of residency in family medicine, and I knew this was a grave patient privacy violation. The physician eventually came in and began to talk to us and to my shock, quickly turned to the x-ray view boxes and directed our attention to the MRI. I had to ask the doctor twice to confirm that that was indeed my brother’s MRI on the wall.
David had a large glioblastoma multiforme in his brainstem. What he was describing as fainting when laughing out loud was pressure being put on the brainstem with Valsalva and shutting down brainstem function. Unfortunately, my prognosis was correct. He had a terrible brain tumor and only a few months to live.
After a biopsy, he received the best treatment at the time for that disease, which was radiation coupled with cisplatin. Futility was obtained quickly and by early June it was clear that he was beyond hope of a cure. He and his wife had their fourth child during this treatment regimen, and he had well over ten thousand people praying for him all over the world through his church’s network, and yet his health continued to decline. My wife and I were scheduled to graduate in July from our residency in Corpus Christi, and after the ceremony, we drove like the wind to San Antonio. David had been on hospice for a few weeks and was near death, slipping in and out of consciousness as we sped there.
When I arrived around 6 pm I saw David in his hospital bed, essentially in a coma, but he lightly squeezed my hand and seemed to mouth what he often called me, O’Kenny.
Sitting around David was his wife, my two sisters, my younger brother, my mother, and myself. We were a mix of somber and comforted, telling stories and occasionally laughing. As it approached midnight with my brother’s death rattle rhythmically sounding, we started recounting the stories of our time in Alaska. We started to tell the story about shouting “Hey Bear!” and laughed about the turtle that was David. We all laughed—the long and hard laugh of a family in pain together.
After a bit, just after midnight, we stopped laughing and settled into quiet. Total quiet, as we all noticed together that David had died.
There is much that is unknowable about the final stages of death. Many hold that hearing is one of the last senses to go, as some who have been in comas and recovered relay things heard while comatose. I believe David’s hearing was intact in those final moments. I believe he laughed, which pushed that pressure on his brainstem over the edge, and surrounded by love and family, my brother died laughing.
How do you want to die?
Do you want to die remembering wonderful moments? You won’t unless you make those memories and eschew working all the time. Do you want to die surrounded by love? Then live loving. If you want to die rich and unmourned, that too is in your grasp.
I want to die laughing.

Prisca Mbonu, Class of 2026
I learned so much that semester. I learned about the different ways a person can fall in and out of love, how to measure specific...
Read More
Prisca Mbonu, Class of 2026
I learned so much that semester. I learned about the different ways a person can fall in and out of love, how to measure specific heat capacity of a metal in Chemistry lab, the perfect step-by-step method to parallel park for my driving test, what medical specialty I would likely end up in after the grueling pre-med years and…about depression.
During that semester, I would become intimately familiar with the illness known as depression.
An illness that I had been largely unaware of throughout my life. An illness that I had brushed aside by the sheer will of what I often call “African stoicism,” a tough outer shell, impermeable to hardships and unperturbed by the twists and turns of life.
Depression? Who is that?
That semester. The lack of appetite. The loss of interest in life. The avoidance of friends and classmates. The skipped classes and missed meals. The unexplained sadness, unprovoked irritability, and unstoppable tears.
All signs pointing towards depression. All signs we could not see. All signs we would not see.
That is, until they became signs that refused to be ignored.
After endless probing and pleading, you finally confide in me. You tell me that you need help. That you have been struggling for a while. That you are sad all the time. That you don’t see the point of living anymore.
The last part breaks me.
You tell me.…you think you might be depressed.
It turns out that while I have had no experience with mental illness, you’ve had far too many. Enough that simply uttering the word “depression” elicits a visceral reaction.
You have experienced the shame and isolation associated with seeking mental health care. You have seen family members live silently with mental illness, afraid of whispered rumors and the inevitable judgement of others.
Unlike you, I did not grow up hearing words like depression, anxiety, and bipolar disorder. I am ashamed to say that I knew nothing about your illness at the time.
But I am determined to get you through this “hurdle.”
Straight A’s. Type A. A perfectionist. High achiever. This is simply another question to answer. A difficult but requisite college course to travail.
I do my research.
Exercise. We walk and walk. We talk and talk. Until our legs hurt and heels blister. Until we have exhausted both our words and our selves.
Diet. No more skipped meals. We are first in line at the cafeteria. A healthy breakfast to start the day. Lots of fruits and vegetables. Don’t forget to stay hydrated, always.
Music. We explore the rich music of my culture. I teach you the lyrics and dance moves. You marvel at the vibrancy and uniqueness of Afrobeats. I marvel at the fact that the music I took for granted could be so deeply appreciated by another.
K-dramas. We watch all the good shows, all the bad shows, and of course, everything in between.
School. We study together at our highly coveted spot in the library. You help me with art projects. I help you with Calculus I.
Everyday we live in this bubble of our own design.
Has the ever-looming cloud of sadness passed? Are you smiling more these days?
Or am I imagining the slight curve of your lips? Do I hallucinate the faint gleam in your hazel eyes?
I must have. Because you aren’t better. Distracted? Maybe. Not better.
We have been pretending that nothing is wrong. But ignoring an illness does not make it go away.
I am crippled by the fear that I can’t help you. That I am not enough. This thought terrifies me.
You are my roommate. Brought together by luck of a random draw and yet, you have become so much more. You are my friend.
I have learned to always push through obstacles, fearless and determined. But this isn’t just an obstacle. Your depression isn’t just a problem to be solved. A thing to bulldoze through with my endless optimism and stoicism. One more adversity to face boldly with my shield of resilience.
I bring up the next logical option. It’s time to seek help from a professional. Therapy, maybe?
You resist the idea. I knew you would.
But I persist. And reluctantly, you agree.
We walk and walk. But this time, we are not simply taking endless loops around a geese-invaded lake. This time, we walk with a purpose. This time, we walk to get you the help you need.
We walk, but don’t talk. Instead, we allow our minds to wander in an odd yet peaceful silence. And then I wait.
Your first counseling session is hard. But week after week, without fail, we continue to go. We continue to walk. I continue to wait. Now we have a new routine.
This time, you truly seem better. I am numb with relief.
Because in those months, I couldn’t tell you how scared I was. Afraid that our efforts would be inadequate. Afraid that you could sense my ignorance about your illness.
Thank you for letting me in. Thank you for getting out of bed at my insistence. Thank you for trying.
And thank you for allowing me to care for you.

Kavneet Kaur, Class of 2023
Character Description Kavneet: A naïve 3rd year medical student working a shift in a rural Emergency Department at the time of yet another COVID surge....
Read More
Kavneet Kaur, Class of 2023
Character Description
Kavneet: A naïve 3rd year medical student working a shift in a rural Emergency Department at the time of yet another COVID surge. Must work shifts for 28 out of 31 days this month. Tired, but ready to work and take on a challenge. Always hopes for the best and tries the see the good in a bad situation.
Scene: It is month 8 of 10 of my Emergency Medicine rotation and delta variant reared its ugly head.
====================================================================
[Cruising down the highway at the crack of dawn with the window rolled down, I let the cool, crisp air wake me up. The radio is screaming on repeat: “The death toll from COVID-19 is increasing day by day… Delta variant seems to have world leaders worried of yet another spike in cases”. As I pull into the parking lot, two deer cross in front of me near the entrance of the hospital. You don’t get that in the city.]
Hour 0
KAVNEET: “How is this shit still going on?” I grumble to myself as I walk over to greet my attending in the breakroom. I notice the tracker board with the list of current patients… just when I thought I was going to have a ‘Q word’ day.
“Q word” means “quiet”, but you don’t dare say that word in the ED unless you want all your staff cursing you out an hour later while being knee deep in patients that decided to take a trip to your emergency resort.
I overhear the overnight attending pass off a patient to my attending physician, who in disbelief remarked “This was the same patient I had on shift two days ago.” The patient is COVID positive and is currently waiting to be transferred to another facility for more intensive care, but no hospital nearby is accepting patients.
They have now been in isolation for more than 72 hours. Imagine a 6-foot by 6-foot room with white walls and no windows. No human contact outside of nurses coming in to give you meds or adjusting ventilator settings. Sedated. Looking more machine than human. Listening to the music of the vital monitor beeping similarly to a ticking clock, amid chaos happening in the room to the left and to the right of you. Lifeless.
It is quite literally the closest thing to solitary confinement without being imprisoned.
My trance breaks as we rush through the remainder of the patient list. I notice there are others waiting more than 40 hours needing to be admitted to the second floor for inpatient care.
Here’s the thing that the public tends to forget- there are still a portion admitted patients in need of critical care, who do not have COVID. This could be your grandfather having his first heart attack, your significant other that just got into a car crash or is having a miscarriage, or your child that is about to slip into a diabetic coma.
And the fact of the matter is that there may not be a place to put them or stabilize them. Even if we can, they are still left waiting for another hospital to “accept” them to get the care that they need.
Why does someone need to be interviewed to see if they are sick enough to be treated? How does that make sense?
Hour 2
KAVNEET: More patients are checking in. COVID patients get priority, especially if they have a below desired oxygen level. In other words, “priority” means you can be put in a room with an actual door that closes. What do we do when those rooms run out you ask? I pray to God. You pray to whatever Higher Power you believe in or just hope for some good vibes. “We have NO rooms open for COVID patients!” I hear the charge nurse scream as if it was not obvious. Though by the look in her eyes, more a scream of frustration than one to state facts. Let those prayers begin. We now have no option but to fill in these makeshift “rooms” with possible COVID patients. Picture a room divided into smaller sections by a shower curtain instead of an actual door. I try to justify it to myself as, “well, it’s not like there is any other place we can put them, and we can’t just stop seeing patients.”
Hour 3
KAVNEET: I do the best I can to help my attending and the staff see patients. At one point, I go to the front to help triage patients, some of whom had now been waiting for at least an hour. Our triage room is quite literally the size of a closet, so you can imagine how this was about to go.
With my head held high, a N95, surgical mask, and face shield, I march into the lobby and scream the first patient’s name to bring them into our broom closet. Yes, scream…it is that chaotic. I ask what brought them to our ED today. Cough, fever, shortness of breath? What a shocker.
“Have you been vaccinated?” I question with skepticism. No? Surprise, surprise. I proceed to get the vitals. Blood pressure 142/94… eh, won’t kill you, temperature 99.8… low-grade fever, heart rate 104… tachycardic, oxygen saturation 92… mildly hypoxic. Yep, this is to be expected. Ok now to swab for COVID.
Like clockwork, now onto the next one.
Hour 3.5
KAVNEET: We officially maxed out on the makeshift rooms, but we still have a lobby full of unseen patients. “What can we do? I understand we don’t have any space to put them, but we can’t turn them away,” my attending physician shouts through his N95 to the charge nurse as he rushes to check on a critical patient that just came in with low oxygen saturation. “PAGE RRT STAT”.
34-year-old female, with oxygen saturation in the 50s.
As my attending and others work to assess the gravity of the situation, the rest of us manage to add two gurneys and a chair… three extra spaces in the hallway of our small boondocks ED. If a code blue walks in through the door right now, we would literally be doing it in the ambulance bay outside of the hospital. Totally code compliant.
I rush back to the critical patient that was brought in. Everything and everyone moved like an assembly line. Prepare the meds, sedate, paralyze, intubate, get out. I open her chart and glance through it. She is a healthy young woman without any health conditions. She has had COVID-like symptoms for 2 days and began to develop shortness of breath overnight. So why is she this bad? Something is not adding up…Vaccination status? Unvaccinated.
As we exit the room, the front door almost knocks me down as the medical director of the Emergency Department darts in through the door. Before I can process, monitors start going off. BEEP BEEP BEEP! The patient that we just intubated… a bunch of staff rush in and one of the nurses’ pages RRT again. Oxygen saturation is 70. I stand outside the room as I see the panic in everyone’s eyes. There’s simply no time for this right now.
My attention diverts behind me as I overhear the charge nurse and medical director calling hospitals from DFW to College Station to find beds so they can move our current patients out to add new ones to the trenches. The medical director even made a personal call to the CMO of the hospital system. Little did I know that in the last several hours, we were still getting calls from the transfer center to accept patients from Kansas.
Hello? What happened to the entire state of Oklahoma?
Hours 4.5 to 9
KAVNEET: We come up with a plan to open a currently unused space on the second floor to put some non-COVID, lower acuity patients. One of the nurses told me this is the first time since the pandemic began 1.5 years ago this was being done. And for the first time since beginning my shift, I force myself to find a moment to stop and take in what is going on around me.
Do you think if an unvaccinated person saw face to face what it looks like to have more than a “COVID cold”, they would change their mind about getting vaccinated?
I often think about that young lady on the vent. If she made it off, her life will never be the same.
On a systemic note, I’m still trying to grasp how we got here? I see nurses, techs, RTs, pharmacists, radiology techs, and physicians running around the hospital trying to do the best they can, trying to solve problems that were created by this system, trying to juggle tasks out of the scope of their practice on top of their normal duties because there is no one else there to do it. I am appreciative of how hard each team member worked in our small ED that day. They are the true embodiment of perseverance and fight.
On top of dealing with a public health crisis, the unfortunate reality of working in a small ED such as this one is that patients are at risk of dying, simply because they cannot get to another facility for more intensive care. Bigger city hospitals will not accept more patients because they are also being bombarded with COVID, and statistics show that most of these patients are also unvaccinated. Even then, at least the bigger hospitals are equipped with resources and specialists to handle the surplus. To put it into perspective how smaller, boondocks EDs are affected, if you are unfortunate enough to come on the wrong day, your options are to talk to someone through an iPad or get transferred to another facility that has someone physically there to take over your care. Often, it’s the latter and we are 40 minutes from the nearest big city hospital.
If being vaccinated means less stories like what you just heard, less burnout for the people who are tirelessly and endlessly taking care of you and your loved ones, less loss of the ones you hold close to you and heck, maybe even you yourself. The question I then pose to you is: If you do not have a legitimate medical reason to not get vaccinated, what is the hesitation to get the vaccine? Whether you are pro-vax or vaccine hesitant, we can all agree that we are mentally and physically tired of this and want life to go back to “what it used to be”.
====================================================================
**This piece was a finalist for the inaugural production of Stethoscope Stage
Sarah Lyon, Class of 2023
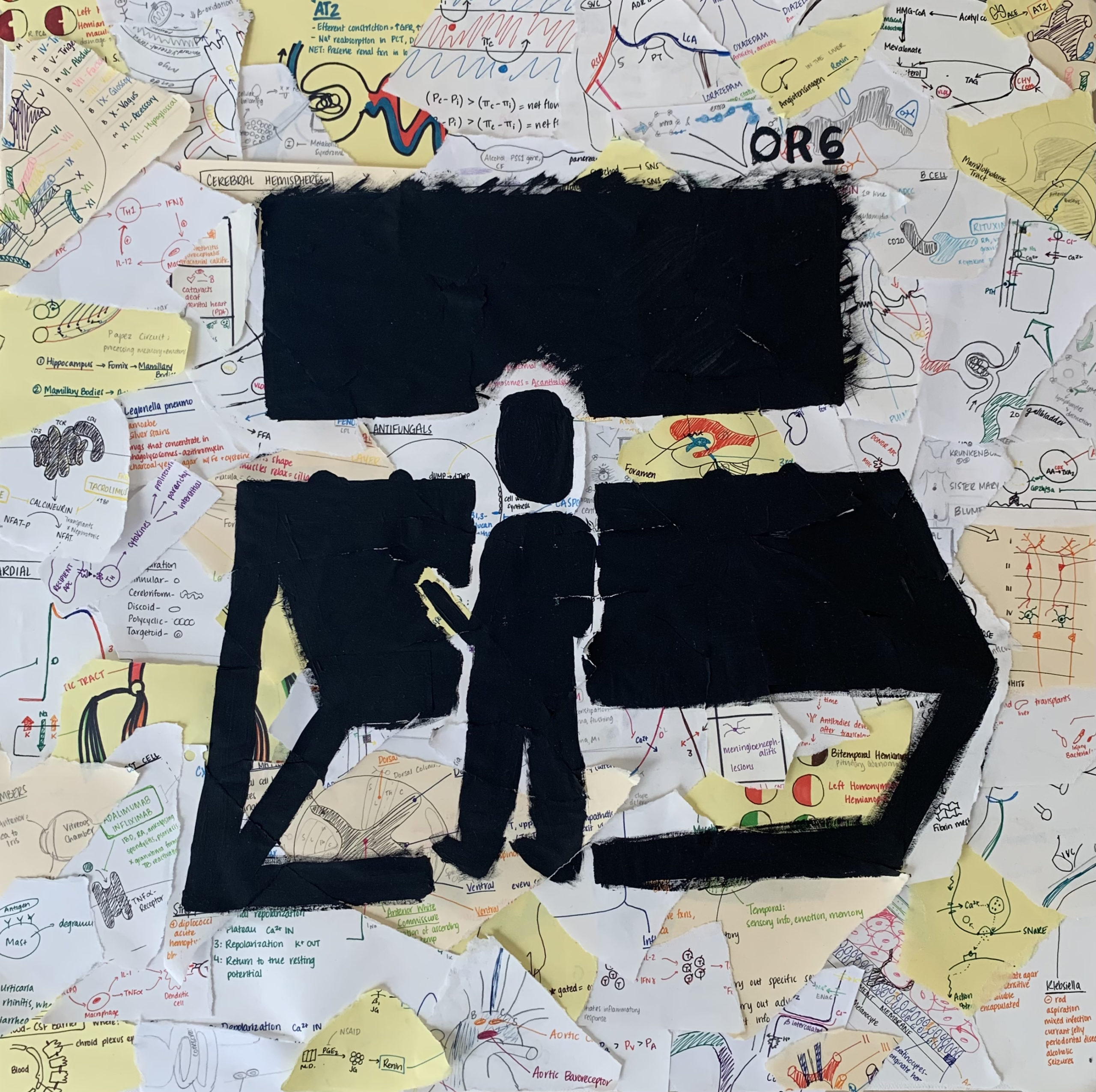
paper and ink, tape, and acrylic paint on canvas A Medical Student’s first time scrubbing into the OR. Snippets of everything they learned during didactics...
View Art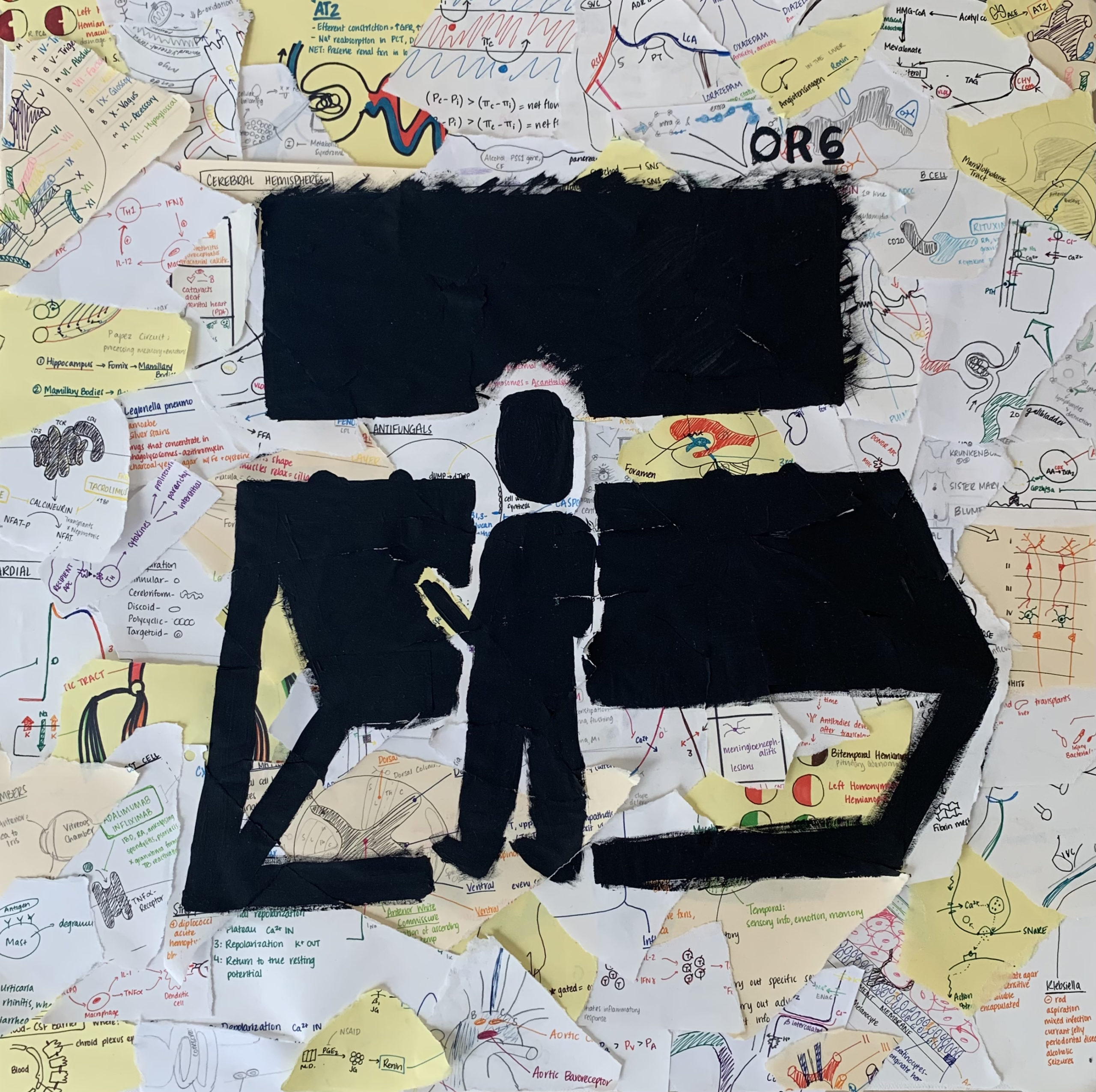
Sarah Lyon, Class of 2023
paper and ink, tape, and acrylic paint on canvas
A Medical Student’s first time scrubbing into the OR. Snippets of everything they learned during didactics flashing in their mind. Looking into the unknown darkness of OR 6, unsure of what is to come. Will they be prepared and competent enough to provide exceptional, empathetic patient care?

Sarah Cheema, Class of 2023
Sometimes I don’t know if I can handle another one. Another uncomfortable pause, another sudden shift in body language, another dance of “did you get...
Read More
Sarah Cheema, Class of 2023
Sometimes I don’t know if I can handle another one. Another uncomfortable pause, another sudden shift in body language, another dance of “did you get the vaccine” and “no, it was too quick,” “no, I don’t know what’s in it,” “no, and I will not.”
I wish it were just a simple question and an answer – like all the other checklists in my patient visits. I can ask a patient about their home life, diet, drug use, and sex life and get an answer so nonchalant I have to double-check that they’re listening. But, the same person might nearly freeze when I ask about the vaccine. It’s almost as if I can see their spine straighten and their muscles tense, prepared for Battle with the Know-It-All Doctors (and their Students). Their walls come up and suddenly we are miles apart. That’s what I hate the most. Not even the uncomfortable conversations, but the sudden distance, the instant formality as if it is no longer two people speaking in a tiny room but instead, a hot-seat interview on a news channel.
This is not to say they are all the same, they are definitely not. There are those genuinely seeking information, truly torn between a desire for safety and a fear of complications unknown. There are those paralyzed not by their own fear, but their daughter or sister’s fears. There are those with bookmarked Facebook posts, ready to brandish a vaccine horror story like a knife. There are those who I wonder about the most. Those who strongly and firmly state “no” and offer no further engagement. Then, there are those who I feel like begging. The 34-year-old pregnant woman, the diabetic 65-year-old headed for dialysis, the elderly 83-year-old in the emergency department. With them, I walk the thin line between persuasion and disillusionment, hoping I don’t trigger the dreaded blank stare. I think of my unfortunate patients. The 31-year-old guy who was finally cleared to go home after a 60+ day hospital stay, only to suddenly pass away from hospital-acquired COVID 1 day before discharge. Sometimes, I refuse to walk the line at all and I simply move on.
Honestly, it all depends on the day. On good days I feel kind and patient, mindful that we all crave the same health and freedom. Other days, I am tired and frustrated. Tired of all the cracks in the system, like the fact that students aren’t supposed to see COVID positive patients yet I spent countless days in the ER listening to the lungs of patients incidentally found COVID positive 15 minutes later. Tired of spending my days as a medical student next to a doctor on a laptop telehealth visit instead of floating between exam rooms as my predecessors did. Tired of the relentless acne from wearing a mask for 8-12 hours daily. On these days, my brain reverts to its primitive schema mode and determines the status of each person: either With Us or Against Us. I know, I know that this is not the reality. I know that everyone supports healthcare workers and vaccine hesitancy is remarkably multifactorial. Still, compassion fatigue is real and it permeates hospital halls like its own disease.
I try to imagine what the vaccine is to them. Often, it seems impossible we are talking about the same thing. What is to them a dreaded and dangerous trap is to me a golden ticket, a precious shield in a chaotic war zone. It absorbed some of the helplessness that we were drowning in. It gave me a guiding light, a dream of an education unmarred by a new virus. The “truth” outside the politics, fear, and hopeful dreaming, probably lies somewhere in the middle. The vaccine is neither a magical cure-all nor a manufactured lie. It is just a little piece of nucleic acid that travels into cells to become a protein that WE HOPE MAKES A DIFFERENCE.
====================================================================
**This piece was selected and performed at the inaugural Stethoscope Stage production in 2022**

Shanice Cox
Written & Performed by Shanice Cox [audio m4a="https://mdschool.tcu.edu/wp-content/uploads/2022/05/Take-a-moment….m4a"][/audio] Take a Moment Chapter I: Obstetrics and Gynecology Take a moment... to breathe Take a moment...to...
Read More
Shanice Cox
Written & Performed by Shanice Cox
Take a Moment
Chapter I: Obstetrics and Gynecology
Take a moment… to breathe
Take a moment…to seize…this moment that sits before you
Take a moment… to see,
beyond the gown, the drape, or the anatomy
Take a moment… to listen to the history,
To the crackles in her speech, to her hesitation,
To the hum in her pause, to her tone’s vibration,
Take a moment… to view
What it is that lies in front of you
As her hand is carefully positioned behind her head,
And the gown is respectfully placed,
while ribbons gently touch the side of the bed,
and the slight embarrassed flush of her face
Take a moment…to view
the contour of her breast
Clockwise and counter
view symmetry, asymmetry,
are you still there?
Or has she become a mindless exercise of your checklist,
color, texture,
Are the nipples inverted,
Is discharge produced,
are nodules immobile,
is her quality of life reduced?
Take a moment… to be silent
With differentials and questions and familial history pooling in the mind,
For you must make space in this stillness of time,
To deliver a news that may shift the course of this rhyme
Take a moment…to reimagine,
That this couldn’t be you,
That you couldn’t be the one
To look in her eyes and deliver the troubling news,
It was the life you wanted,
The only specialty you knew,
But over the course of your training,
The weight of this burden grew,
Take a moment…to revisit
Those feelings that once were,
Filled with such promise,
That now feel so obscure,
Take a moment…to gather
Your thoughts,
your desires to serve in this space,
To counsel, to teach, to empower, and to share a thoughtful embrace,
To right the wrongs of centuries-old medical practice
With dignity, humility, and grace
You approached the field,
With only the thoughts of positive outcomes,
But failed to consider…when there wasn’t one,
Your story did not capture the woman who fell ill,
Or when the fetus had been delivered,
Cold, pulseless, and still
Take a moment…to process
How you revered in maintaining the health of the womb,
But after seven days on the service,
This vessel of life,
Evolves into a hollow, pear-shaped tomb,
Take a moment….to reconsider,
What life would be if you made more room,
To till the soil of your garden,
And allow for the seeds of destiny to bloom,
Take a moment…to look
Into the mirror and see what you’ve become,
Because there in that reflection,
There is a slight resemblance of someone,
Fragments of the old, but glimpses of the new,
Moments that reflect past passions,
but notes of what they had morphed into,
This desire to serve extended farther than that of the woman’s womb,
And in this infinite Eden of possibility,
My brainchild found room
Chapter II: Urology
Take a moment…to reset
To look at this rotation anew,
Because what you had been searching for,
had somehow found you,
It began with a knock on the door,
And a sheepish reply “You may enter”
Unconsciously I shift my attention to the woman,
But she is not who sits at the center
Take a moment…to view,
The air of defeat in the slouch of his posture,
Take a moment ….to recognize his courage to seek a doctor,
He peers up at you,
An emptiness in his gaze,
His wife quickly rushes over to hold his hand,
To somewhat mask the depth of his dismay
He tells me of their journey,
And how they’ve tried for years and years,
Until they sought the help of medical professionals,
Who would somehow ease their burgeoning fears,
He spoke of her strength,
Navigating conversations about her ability to conceive,
He spoke of her courage,
To defend and protect her family without reprieve,
Take a moment…to notice
The pain that continues to resurface,
And all that they had been through,
The waning support of their loved ones,
The constant judgement and ridicule,
Yet she sought answers,
she completed all the tests,
But when they all came back normal,
She entrusted him to do the rest,
Take a moment… to breathe
Take a moment…to seize…this moment that is before you
Take a moment… to see,
beyond the gown, the drape, or the anatomy
Take a moment… to listen to the history,
To the crackles in his speech, to his hesitation,
To the hum in his pause, to his tone’s vibration,
Take a moment… to view
What it is that stands in front of you
As his hand is carefully positioned atop his head,
And the gown is respectfully placed,
while ribbons gently touch the side of the bed,
and the slight embarrassed flush of his face
Take a moment…to inspect
the meatus and penile shaft,
Testicle, epididymis, spermatic cord,
Give yourself this moment to perfect your craft,
Are the testes symmetric,
Is discharge produced,
Are prostate nodules immobile,
Is his quality of life reduced?
Take a moment…to reimagine,
That this could be you,
That you would someday be the one
To look into his eyes and deliver the hopeful news,
It was the life you wanted,
Combining the admiration of a specialty you once knew,
Yet a new seed was planted,
With a flourishing destiny coming true.
====================================================================
Artist Statement:
This piece is dedicated to my grandmother, Claudette Cox-Brown, who exposed me to the intricacies and
delicacy of reproductive health. She served as a nurse midwife in Jamaica, England, and New York and shared with me so many
precious narratives of femininity, obstetric care, and the hardships of navigating pregnancy whether wanted or unwanted in
years past. Over time, the initial intrigue of her stories sparked an interest to pursue a similar path, and it followed me for a large
portion of my life. It paved the way for research opportunities in college focused on breast cancer, a medical mission’s trip to
Durban, South Africa focusing on the obstetric care of mothers and babies affected by HIV, my first career as a medical assistant
at an OB/Gyn office in Washington DC, and even the acceptance of a medical fellowship whilst in medical school, and for that I
am truly grateful.
However, this dream of mine to be an OB/Gyn never included the emergencies that happen in the delivery room. And
when things go awry, it happens fast. In my many experiences, I had always seen the outcome of healthy mother and healthy
baby, but never considered the possibility of losing either. My time in the longitudinal clerkship exposed areas of my journey that
I seemingly avoided, or hadn’t been privy to, and placed me in an emotional headspace I couldn’t escape. The beloved field that
had my heart for so long, had cemented wounds that had me question what the next step would be. In this poem, I address
some of those hardships, but also this love that I have for reproductive medicine transforming into something more, something
that created a space for old passions, but hopeful futures.
Urology has been that great awakening for me, not that I had slept through the life of undergraduate medical
education, but just an opportunity to see things both old and new with renewed purpose. Traits and behaviors that I had
perfected in my pursuit of being an obstetrician, have crafted my mindset about practicing urogynecology. I feel hopeful that my
interests in gynecologic procedures that focus on health after childbirth such as pelvic floor instability and urinary incontinence,
along with surgeries with the intent to tackle conversations that have are attached to social stigma such as female genital
mutilation and transgender medicine, can be cultivated in this field.
This poem takes you on that journey with me, the journey of facing those emotional hardships with the patient, and
within myself. Take a moment was written as my reminder to find some time, even just for a brief moment to be in that moment.
It is a mantra I use to escape my racing thoughts, to reconnect with patients, to observe, to reflect, and be mindful of the here
and now and sacredness of the space that my medical journey has afforded me. Take a moment though dedicated to my
grandma is a thank you to each obstetrician/gynecologist, midwife, nurse, charge staff, medical assistant, phlebotomist, practice
manager, and sanitation engineer that inspired and prepared me to seek and gain knowledge about every aspect of feminine
health. It is also a commitment to each urologist/urogynecologist, resident, and therapist who have accepted, mentored, and
exhibited patience and support as I worked to figure out the journey that lies ahead.

Shelby Wildish, Class of 2023
Character Description: Medical Student. Female. Late 20s. Eager to learn medicine, self-critical about self-expectations, general baseline tiredness. Wearing hospital issued scrubs, white coat, old worn-out sneakers....
Read More
Shelby Wildish, Class of 2023
Character Description: Medical Student. Female. Late 20s. Eager to learn medicine, self-critical about self-expectations, general baseline tiredness. Wearing hospital issued scrubs, white coat, old worn-out sneakers.
Scene: In Medical Student’s apartment living room. There is a big, colorful, soft chair with armrests in the middle of the room. Beside chair there is a standing full-length mirror. In walking distance from chair is a table, with a lamp, a cell phone, and a laptop computer. There is a rug on the floor and a small footrest.
====================================================================
[Enter Medical Student – she walks towards a chair, stops, turns to face mirror. She looks exhausted.]
MEDICAL STUDENT: You did it. You’ve made it to the end of another busy day. (Moves to sit down in chair, pauses to look down at feet) Damn, my feet hurt. I don’t know how Dr. Barterman does this all day. Walking up and down those long emergency room hallways, never getting a chance to sit down. It’s her shoes, has to be. She has some of those fancy clogs I’ve seen other docs wearing. I need to get a pair. Well, one day…(looks at old sneakers, then up at audience, shrugs)…when I can afford it.
Time to reply to the messages that came while on shift. I bet it’s the college roommate group chat blowing up about the recent girl’s Facetime chat. Another hangout without me; more group memories made without me. I find it interesting how quickly during quarantine it became the “norm” for social interactions to be almost entirely through computer or phone screens. Just shows human adaptability I guess… (Sits quietly, scrolling on phone, to self) I don’t even know what the update is about Amanda’s baby or Susan’s postponed wedding plans. I really need to call them – add that to the long To Do list.
(Looking at phone, slowly smiling then laughing aloud) I can’t believe they remembered that story! That was so long ago.
(Directed to audience) So, once I was dared to jump in frog fountain and then slipped while on the wall and fell face first into the water. (laugh, looking back to phone, nostalgic) we were all such idiots in undergrad. Such fun, but such idiots. I wonder what brought that up in the chat? (directed to audience) It feels good not to be forgotten. I remember this one time that Amanda, Susan, and I snuck into my brother’s house and stole his car during a snowstorm. Us three freshman girls, just trying to do some car drifting in the supermarket parking lot. I definitely need to remind them about it. (start typing on phone, to self) Too funny. (phone dings with notifications, medical student sits quietly, smiling and typing replies to the group chat.)
(Smiling, student puts phone down, looks off into the distance, demeanor changes to one of concern. Look around room, pick up phone and begin typing)
Guys, did you hear about those mass graves for unclaimed patients on an island near New York City?
(sits quietly)
(Irritated, speaking to audience) How can I be laughing when such things are going on in the world? I should be reminding my friends about the situation at hand. Bringing the conversation back to the patients, back to the families, back to the healthcare workers and back to COVID-19. (stand up, pacing and talking to self) Remember your reality. Remember the world’s reality. You wake up each day, and are reminded through new articles, research journals, social media posts, videos, and patient stories of the one sole focus – COVID. Don’t forget it has caused schools to close, businesses to shut down, economies to crash and nations to close their borders. It has caused millions to become unemployed, thousands to become overworked and all to become fearful. It has killed. It is killing. And it will continue to kill.
How dare you laugh? How dare you forget momentarily. (phone dings, student walks back over to the chair, glances at it, reads it, places it face down on armrest of chair, without replying.)
And you, you underestimated this virus’s capability, initially nonchalantly saying {in a mocking voice} “Oh, it’s just another influenza-like infection.” You felt a need to have a reassuring answer for concerned family members. When really, what you should have just said: “what do I know, I’m not even finished my second year of medical school.”
You incorrectly, and almost arrogantly, claiming it only affects the elderly and immunocompromised. Have you temporarily forgotten that you have three grandparents? Think of Nana, of Papa, of Grandma. This virus could take them from you. You are guilty of blissful ignorance. How lucky are you to be so far disconnected from any serious, immediate personal consequences that you have the luxury of having moments where you forget about everything, all things COVID-related. You’re lucky. Your family has been safe. Many families can not say that.
(walk slowly back to the chair, sit-down, pick-up phone and begins speaking while typing) The first patient this morning was a pleasant young guy, maybe 30. (To audience) Not that bad looking either. (back to phone) When we saw him, he was making jokes, laughing, even flirting with nurse Kelly… But you could tell he was having a really hard breathing. (To audience) His face was so pale. (back to phone) We got his oxygen levels. It was 86%. Dr. Barterman thought it was COVID and admitted him to hospital. That’s bad news.
(put phone down, stand up, start walking over to the table, stop, to audience.) At the end of the shift, we heard he wasn’t doing well. They found pneumonia in both lungs. He would probably need to be put on the ventilator. And the crazy thing, he doesn’t have any chronic medical problems. He runs marathons. He doesn’t do drugs, doesn’t smoke. He hangs out with his friends, has a dog. And before the quarantine, loved exploring the city. He is a healthy guy. Well, was a healthy guy.
Was a healthy guy.
(continue walking to table, pick up computer. Walk back to chair, sit down with closed laptop on lap.)
I can picture him, before all this COVID stuff, with a group of friends at a brewery. Joking around, laughing. Maybe even having one of those moments when you laugh so hard that you almost fall off your chair in joyful pain. I bet he is the type of guy that looks for the good in the moment. I bet he would tell you not to beat yourself up about reminiscing, almost as if encouraging you the laugh. You feel the sad, the guilt, the hard times, he would want you to feel the good too.
Isn’t that human nature? To feel. Emotions protect against apathetic eyes. Apathy has no past to base experience on. From feeling nothing for nothing, is no life at all.
(pause, look off in the distance for a while. Then re-center, and open laptop, click on a few buttons, slowly read out loud as if reading from phone) The FDA has approved the COVID-19 Pfizer vaccination.
Could this be it? A light at the end of the tunnel. A chance to get some element of normalcy back in life.
(stand up, beginning dialing on the phone, lift phone to ear, pace around) I have to get it. I need to get it for my family, for my patients. I need to get it so I always remember. Remember what COVID has done… what COVID is doing.
Hello, Dr. Barterman. Hi. It’s me, Savannah… Yes, I just saw the news article… I know! … Yes, it’s all so exciting! … It’s what we were hoping for… I can’t wait for when I can get it. Can you help me register? … Great, thanks … Of course I remember him… he what? … when? … Thank you for telling me.
He was healthy… was.
====================================================================
**This piece was a finalist for the inaugural Stethoscope Stage production

Patrick Powers, Class of 2024
Sometimes, it is nice just to sit and listen to the wind rustle the leaves. The cooling temperatures linger in the air like a prelude...
Read More
Patrick Powers, Class of 2024
Sometimes, it is nice just to sit and listen to the wind rustle the leaves. The cooling temperatures linger in the air like a prelude to the winter ahead. I never thought I would find myself here, and I cannot help but smile through tired eyes. How many times have I missed the movement of life around me because of the movement around me? The enigmatic distractions surround us, poisoning the purity of the simple beauties of life. I admire the leaves in the fall. Of course, their color change inherently captures my attention as a reminder to stop and ‘smell the flowers,’ in a similar way a set of olive-green eyes might remind me to sleep, remind me that I have to eat three times a day, to try not to clench my teeth, and that, really, it will all be ok. In the end, there is an undeniable elegance to the falling of the leaves; a gentle but self-assured poise to each and every leaf that, when the time is right, plucks itself from its roots, and bravely sets sail on its solitary, yet sui generis voyage. The time must come for all leaves to embark on their journey, and though the trek may route through a previously undiscovered, and albeit, arduous, path, just as one cannot stop the leaves from changing colors, this too, embraces its own inevitability. How valiant, to stare down the fear of falling, to trust the make of their ship, to sail alone. Their destination is clear, their conviction clearer. The winds may blow, swaying their ship, aggressively rocking the foundation in an unrelenting manner. But, clever as the leaves are, flow with each windy blow, like water around a stone, never deterred from their ultimate goal, but ebbing gently with each test from the wind. No matter how hard the winds may blow, how laborious each challenge may appear, or how many bruises each leaf must endure, just as one cannot stop the leaves from changing colors, this too, embraces its own inevitability. As the leaves quietly, yet confidently, make their way to the ground, leaving behind the branch which had been their home for so long, so too must we all embark on our own journey. Which then begs the question, what is the ground? What is the ultimate destination? Worry not, the end is neigh. Rather, memento mori, only in as far as it gives purpose to life. For what is light without darkness, peace without war, and love without hate.
Perhaps I, too, can learn to be more like the leaves. The fears seem insurmountable, of being left behind on the tree, of falling, of never having the grit to jump when my time comes, of oblivion, cascaded by volume of inexplicable worries that flood every available space in my mind. I am sure the leaves feel similar. How beautiful that expedition must be, though, I think to myself; to experience those tests of life. The wind, with its capricious and fickle self, brings the blowing challenges that provoke us to breathe deeply and suck the marrow of life with each deliberate adventure. We are all meant to thrive so Spartan-like yet gentle, as the leaves do, staring deep into the eyes of falling, knowing we were made to live the life set forth in the path that is unraveling itself before our very eyes, that the make of our ships can and will endure the journey, and to jump, bravely and boldly, heart racing, with a smirk. Perhaps that smirk is to spite the inhibitions, perhaps it is because of the joy of finally jumping from our branch, or perhaps both. Sometimes, it is nice just to sit and listen to the wind rustle the leaves. I cannot stop the leaves from changing colors, and I cannot stop the fear that lingers in my mind. When I think about it, none of that even matters. My heart could flutter, butterflies flapping in my stomach, as I wipe the sweat from my brow. What matters is that we jumped anyway. We jumped off our branch, flying into our odyssey, highs, lows, and in-betweens, tears, laughs, and far too many unforgettable memories to recount, living the life we were meant to live, so that when it comes time to meet the ground, we will not discover that we have not lived. So here we go, with ill-fitted blue scrubs, a set of scuffed-up clogs, and a little too much caffeine, I catch a glimpse of myself in the sliding front doors of the hospital; tired-eyed smile as I sneak back into the resident’s lounge, just a leaf, riding the wind.

Peter Park, Class of 2025
When I was little, I spent my pre-teen summers with my grandfather in Korea. He was a retired salesman who spent his time coaching the...
Read More
Peter Park, Class of 2025
When I was little, I spent my pre-teen summers with my grandfather in Korea. He was a retired salesman who spent his time coaching the local high school soccer team. In the hot, humid summers, he would coach me in an equally intensive sport: gardening. His backyard spanned half an acre of trees, ferns, and cabbage. But his most labored love was his grapevine. Together, we built fences eight feet tall, allowing for her to expand her leaves reaching for the sun. She protected me from the heat like green clouds in the sky, dropping sugary fruit from the heavens.
One day, my grandfather handed me garden sheers with large rusty blades. He said we would prune vines that day. Unsure of what pruning was, I followed his direction: cut each branch he pointed at. My sheers would slice the darkened bark and reveal a white-greenish core, where glistening sap dripped at the center. The grapevine’s branches would fall to the floor with a thud and all the grapes would scatter like marbles.
My grandfather pointed to various branches of the vine, “This one is infected. This one has been eaten by insects. This one is too small.” I nodded with each response but could not understand the differences between the branches we cut and the ones we spared.
We came onto a large branch that was sturdy and strong. Its bark was like the thickness of a tree and would not break under my grandfather’s bare hands. I prepared to move on to the next branch until my grandfather placed his hand on my chest. He pulled me to the branch and said
“Look, it’s dying.”
I was confused. “How? It’s so big. It must be alive.”
He considered, “You’re right. It is alive and growing well. But, if we allow this one to grow, it will steal the energy from the main branch, and go in a different direction. That’s not where we want to take it.”
For the first time, I saw the grapevine as one connected system, and I understood. This sturdy branch deviated almost exactly at a 90° angle. Like a rebellious teenager, she wanted nothing to do with her parent. Allowing this one branch to grow meant the entire grapevine would die. Her growth would be her downfall.
My grandfather noticed my childish stubbornness and assured me that this was for the whole grapevine. It’s better this way. Not wanting to cause trouble, I moved on and began to squeeze with all my might to cut this rebellious branch.
Snap!
Fluid began to pulse out of the old artery with an almost desperate will. I put away my scalpel and began to sheer away more of the fat deposits surrounding the heart. Years later, in the cold air of a cadaver lab, the grapevine had taken shape, manifesting itself into an aorta branching into its capillary beds. I dug a blunt tool underneath an artery, pulled it towards the surface, and deciphered its Latin name: External Carotid; Subclavian Artery. As I followed the arterial branches, I snapped the artery in two, suspended in air with no grapes to fall.
Once again, I viewed all the blood vessels as one connected system, and I understood. My cadaver died from a stroke, specifically from cancer that had both blocked the brain’s artery and redirected new arteries for itself. This was the sturdy branch who became greedy, stealing the energy from the main branch. Her growth became her downfall.
That night, I got a call from my family stating that my grandfather had passed. He had died in his sleep. We learned that “dying in your sleep” is most often because of a dysfunction of the heart, that, for some reason, simply ceases to pump.
You would think that his body might have learned from his years of pruning. That he would know which branches were to be cut and which were to be spared. You would think that I would have remembered to return his calls.
I wondered who would care for the grapevine now. How she could grow without her pruner? Would she meet the same fate as my cadaver?
Many years ago, I asked my grandfather, “what will happen when the grapevine dies?” He turned to his vineyard and reached out, picking off one of the green grapes. He showed it to me, “Even if this grapevine falls, its sweet grapes scatter out leaving sweet memories with everyone who eats it.”
He tossed the grape in the air and I caught it in my mouth. The taste of sweet memories.

Henri Levy, Class of 2024
The man on the table was a stranger to me as many patients tend to be in healthcare. I had never heard his voice nor...
Read More
Henri Levy, Class of 2024
The man on the table was a stranger to me as many patients tend to be in healthcare. I had never heard his voice nor seen him awake. He was already prepped and draped in the typical sterile fashion ready for his liver transplant. Although I had never met him, I knew several scraps of information about this person. I knew that he had a MELD score of 39; without this new liver, he had over a 50% chance of mortality within the next 3 months. I knew that this operation had the potential to extend his life by many years, decades even. I knew his family was waiting to hear how the surgery went.
Approaching the table, I examined the yellow stomach sticking out from the blue tarp marked with a large, backwards L indicating where the incision would be made. Steel and electricity unceremoniously made short work of the previously untouched muscle, fat, and blood vessels. The surgeons peeled back layer after layer, made suture after suture to control the destruction they were causing to extract this rubbery, bumpy liver. This was not my first time spectating during a surgery–nor will it be my last–still, I could not help but wonder about the role of pain in medicine as I watched these well-choreographed events unfold. How could therapeutically hurting a patient play into the role of being a healer?
I think everyone who goes into medicine wants to help people who are suffering. The idea of being the source of that suffering seemingly goes against the vow of beneficence and non-maleficence providers take. In a much less theoretical sense, it makes me uncomfortable to hurt someone even with good intention and sound reasoning. Take, for instance, minimally invasive surgery. We are told that laparoscopic procedures are lighter on the body and yield quicker recovery times. I remember one patient describing feeling like he was just beat up by a bunch of baseball bats after his robotic gallbladder removal. Statements like that put larger, more aggressive procedures into perspective on how a patient feels afterwards. Imagine how someone must feel after an hours long open procedure — the kind with midline incisions that are the full length of the abdomen. This does not even include the anxiety someone might feel just having to go into the operating room for a surgery. Suffering is not limited to surgery either. Medicine is rife with discomfort and pain due to various procedures that range from benign to absolutely life changing. Range of motion tests cause patients with rotator cuff injuries and muscle sprains to wince. Medications we may prescribe can have severe side-effects. It is not uncommon to break life changing news to patients and families causing stress and psychological suffering well beyond just one individual. Inducing some level of discomfort for the patient is common as a physician. Yet all of these, and more, would be considered standard practice. It seems that many of our solutions require things to get “worse” before they get better.
Perhaps what makes this whole concept so strange to me is the idea that it will not be long before any one of us in my class will be expected to do these things. I find myself wondering who am I to inflict this pain on someone? I am just one human in a room, hoping to have letters behind his name someday, trying to practice medicine on another human in the room. In any other context these incisions, maneuvers, and causing general psychological stress could be deemed illegal or at the very least unethical. In a hospital they are expected. Patients trust doctors to do what is best – even if that treatment comes at significant personal cost. That burden becomes even heavier when realizing that there will be suffering no matter what happens. The question is just how much will occur. The 4-year medical school curriculum and 3-year minimum residency training are both testament to the fact that these practices and procedures are anything but random. The gold standards are tried and true in improving people’s lives. We will all be highly skilled after our training is complete – a knowledge built on an infinite series of trials and errors. Still, despite the current triumphs in medicine, outcomes are not always predictable despite a physician’s best efforts.
I saw firsthand how extreme this iatrogenic suffering can be. Unfortunately, this liver transplant case was one of the rare instances where the patient did not survive the procedure. He tragically expired on the operating table despite enduring more than five hours of surgery and multiple rounds or brutal CPR. He did not even get to use his new liver since blood flow was never established. Seeing that chaotic scene will stick with me forever. No errors were made. Everyone involved was highly skilled and competent doing the things they have done hundreds of times before with great success. Seeing everything unfold opened my eyes to just how little a non-medical person knows about the almost violent nature of medicine at times; ignorance is bliss. Liver transplants have a high success rate. 75% survive the first five years after their operation. This is a marked improvement from the mere months this man had without this donor organ. As with any procedure though there are implicit risks that need to be balanced with any potential gain. There were high stakes with the procedure. The decision to proceed was the correct one; to get this new liver was to live for many years to come. Yet had the family known he would not survive, or had they seen the extent of the damage inflicted on his body from advanced cardiac life support, perhaps they would have simply chosen to enjoy those last few months with him instead. Hindsight is always 20/20. It may have been his alcoholic cirrhosis that brought him to the table, but it is hard to shake the feeling that it was medicine that killed him.
Stitching up a recently deceased person is a strange sensation. Perhaps stranger though was the sense of closure it offered with the situation. Medicine is not perfect and our means to achieve our goals can be savage. Yet, we are doing our best with the odds ever stacked against us. We work hard to ensure that people suffer to the least extent possible. Situations may go from bad to worse, but the intention is there and the knowledge and skills backup every decision that is made. Yes, suffering is inevitable, but surely it can be minimized. Just like with this man before me, the sutures were a feeble, but well-meaning attempt to make things better. Ultimately, it makes me think about the role of striving to do better as a physician and a person. At the very least, he will be presentable for his family to see him one last time.

Matthew Pagano, Class of 2024
A mother and son duet. Mom draw her staff, Linea nigra noting her fertile tune Blue lines track his song, and purple hers. Yellow...
Read More
Matthew Pagano, Class of 2024
A mother and son duet.
Mom draw her staff, Linea nigra noting her fertile tune
Blue lines track his song, and purple hers.
Yellow contractions, thunderous cymbals
Time for the concerto to close, burgundy drapes to be drawn
and a new solo to begin.
Intermezzo
Blue absence
He won’t play, their performer is listless
a much crasser show must begin.
Hands clasped, like sterile prayers given
Mentally reciting verse from text, medical bibles.
Expectation of what is to come.
Human hope to be the unwritten exception, an unforeseen statistic.
Gospel gives way to staccato
cutting
ripping
tearing
and
Silence.
no cry, no croone.
Red, iron metal, bloody, crimson afterbirth
A former home, the drumming of maternal’s love
a welcomed cacophony
giving way to
Silence.
still.
discarded tissue.

Tom Deas, MD, Physician Development Coach
Resilience by Peggy Godfrey No promises the wind will make Unto the tender grasses Nor leave a trace or memory Nor count the time that...
Read More
Tom Deas, MD, Physician Development Coach
Resilience
by Peggy Godfrey
No promises the wind will make
Unto the tender grasses
Nor leave a trace or memory
Nor count the time that passes.
In gentle breeze or howling storm
Passion ebbs and flows
Resisting not, the grasses bend
Tremble, sing, and moan.
Without the wind the grasses
Never have a chance to know
Their grace or range of motion
Songs of joy or woe.
As though in battle with the wind
The lifeless creak and grown
Stiffly clattering in the breeze
To break beneath the storm.
But, oh, to watch the living
Bid welcome to the wind
Wind and grass so separate
In union once again.

Peggy Godfrey is my exceptionally talented sister, Colorado rancher, and respected cowboy poet who has published four collections of her authentic cowboy poetry and prose including Write ‘em Cowboy (1993), Write ‘em Roughshod (1994), Write Tough (1995), and Stretchmarks (2003). Resilience is one of my favorites. The visual and auditory imagery of the grass and the wind reveals Peggy’s keen observation of nature and awareness of her environment. More importantly, she reflects on her life experiences which have ebbed and flowed as the grass bending in the wind. Her lyric captures this certainty: without stress, we cannot develop our full potential of “grace or range.” The weak, rigid, and inflexible, unable to learn and adapt, will fail in the storm.
Resilience is the ability to endure, recover, and grow stronger in the presence of adversity. All worthy endeavors, especially medical school, residency, and the life-long role of physician require resilience. We confront adversity and endure; face failure and recover; accept the “no’s,” adapt, and become stronger. Brilliance and skill alone are insufficient to sustain us through training and medical practice. Like the grasses, we must “bend, tremble, sing, and moan” to find our “grace or range of motion” in our “times of joy or woe.” It is no coincidence that Coach Thu and I are paired in Team Resilire. My sister and I were truly blessed, as children and well into our adult lives, to learn to be resilient from a father who lived to 104 years.
Our father was the personification of “The Greatest Generation” and a gold standard role model for resilience. He was a small-town boy from Arcadia, LA, who in his teens endured The Great Depression of the ’30s. He attended Louisiana Tech at the age of 16, playing football and boxing. He subsequently attended medical school at LSU School of Medicine in New Orleans where he met “Scooper.” They married in 1941 – the same year he was called up to serve in the violent WWII battles in the Pacific. He served as a front-line physician in the Philippines Islands. Despite the grave adversities of war, he advanced to Regimental Surgeon and earned the Silver Star, Bronze Star, and Presidential Unit Citation for leadership and uncommon valor saving wounded soldiers under fire. Later in his life, he treasured the reunions with “my boys” the dozen or so remaining medics who were in his command during WWII.

After the war, he completed another two years of residency training before becoming a family physician in Homer, LA in 1947. (Tom, Jr arrived in 1948.) It was a difficult and demanding life of frequent house calls day & night, superimposed on long hard days in the office and hospital. In establishing his medical practice and as a community leader and moral voice, he faced adversities with wisdom and grace—enduring, recovering, and growing stronger.
As a child, I felt no calling to medicine – a difficult profession that demanded so much of my father. I recall thinking, “I never want to work that hard.” However, he thrived in the joy of his intense physician work-life. He was also a prolific writer, reflecting often in prose and poetry on life’s joys and sorrows. His reflections encompassed his World War II experience, my mother – “Scooper,” the love of his life, family, and his role as a small-town family physician, community leader, and man of faith. His passion for medicine, joy in his work, and his unconquerable resilience were ultimately the reasons I altered my choice of profession from research chemist to physician four years after college graduation.
Here is an excerpt from a letter I wrote him in 2014 when he was 98-years-young and I was just a kid of 66:
Dad, I cannot tell you how much it has meant to me to have you as a model of a caring physician devoted to your patients and profession. I share your enthusiasm for the diagnostic challenge. It has been such a satisfying career. I cannot imagine my life if I had not found my way to medicine. For that, I am most grateful to you and your great example. I treasure the notebook that you prepared in 1946 to start your practice which summarized the current therapies of the day. A chair from your office waiting room is in my home study to remind me of your successful medical career as a beloved family physician.
My Dad died in May 2020 at the age of 104, my father, my role model of resilience finally let go. He died peacefully in his sleep of unknown causes and in perfect health. I would have described his cause of death as “resilience exhaustion.” He left this verse in reflection, his variation on Tennyson’s Crossing the Bar.
Sunset and evening star,
When I put out to sea
When I go across the Bar,
I want no tears for me.
For I am very much alive,
Though I lie with unseeing eyes,
I lie not dead…
I am forever thankful that he gave me his name, his profession, and his resilience which does indeed live on.

Thomas M. Deas
1916-2020

Helena Kons, Class of 2023
After three months of excruciating hours, ailing patients that had been stuck in the hospital for weeks, and intimidating attendings who peppered us with questions...
Read More
Helena Kons, Class of 2023
After three months of excruciating hours, ailing patients that had been stuck in the hospital for weeks, and intimidating attendings who peppered us with questions out of the blue, the transition to outpatient has been smoother, calmer, and, well… Boring.
Rather than rounding on patients with appendicitis, sepsis, or aspiration pneumonia as I had during my time in the hospital, I am now doing medication reconciliation, hand holding, and counseling – So. Much. Counseling. While I’d always loved talking to patients, I find myself constantly having to redirect patients to the questions at hand to prevent them from getting sidetracked. Half the time I feel like I am learning how to be a therapist instead of a physician.
This lament is what is running through my mind as I’m sitting in my oversized white coat in my preceptor’s office, glancing absentmindedly at the ever-growing stack of papers on her desk. I’m thankful, yet again, for the surgical mask on my face that hides my occasional subtle yawn when she walks in.
“Helena, I have some bad news to share.” She is looking down at her desk, her shoulders drooping beside her. Even as someone who is training in medicine, I find her words so doctor-ish.
“Okay,” I say, a little distracted. I had been going over my to-do list in my head. Pick up the groceries on the way home, 100 more flash cards, 20 practice questions…
I take a deep breath of the stuffy office air. I have been yearning for the pace of the hospital. I missed constantly seeing patients and scrubbing into surgeries. Lately I’ve found myself agitated at the idea of spending 40 minutes with the same patient. ‘I miss just getting to do medicine all the time’
“Mr. Smith has died.”
A jolt back to reality. “That’s terrible.” I mumble. A reflexive response. But it is not before long that my mind is reeling. Mr. Smith was my panel patient—I had been assigned in my first year to follow him throughout his medical journey. I’d accompanied him to appointments, gotten to know his family, and called him regularly to check in. I was in the room for his diagnosis. I watched as he stared in disbelief upon hearing that he had metastatic lung cancer. “But I’ve quit smoking!” he’d said, “All of my last scans were normal!”
I remember his oncology appointment. I remember how rushed it all felt, and how it was to sit with his daughter in the waiting room. I remember her telling me about her son’s hobbies and her pet’s names and her father’s pride in being the patriarch of their family.
I also remember wiping away tears as I drove to my afternoon clinic. I remember missing questions in all of my other clinics because I was so distracted. I remember missing sleep as I tossed and turned, wondering how much time he might have left.
Most of all I remember feeling angry: at cigarette companies; that I was assigned to such an emotionally heavy case. Angry at myself for not being better at compartmentalizing.
This moment highlights the schism between the fantasy and the reality of being a medical student. In medical school, you inevitably become the recipient of a hefty amount of praise that you’re not entirely sure you deserve. The myth goes that patients look up to you, your friends from high school envy you, and family members gush with pride at reunions, showering you with compliments about your intelligence and dedication. In a lot of ways, you are society’s idea of perfect. You are young, successful, intelligent and hardworking – many of America’s most highly valued ideals wrapped into the two-word title — “medical student”.
Then there’s the other side of being a medical student that only you, your classmates, and your family members will understand: the constant pressure to be perfect. The pressure to make it look easy. The fear that if it’s already this hard, it will only get harder. The assignment you missed because you only got three hours of sleep for the fourth night in a row. The messy, run-down apartment with dishes that have been in the sink for God knows how long. The feeling of never having it together and never being good enough. It all serves as a constant, sobering reminder: you are anything but perfect.
As we progress through our career grappling with these personal demons, the human aspect of medicine often fades into the background. But today in my preceptor’s office, it calls me back. The first day I met Mr. Smith was perhaps the worst day of his life. I was sitting in the same seat in my preceptor’s office six months ago when she had looked up at me and said, “We have a patient coming in today, and his last CT showed metastatic cancer. We don’t know the origin of the cancer right now, but the prognosis doesn’t look good. I am referring him to oncology.”
I tensed up as I pictured myself in the room watching her give the news. I hated the thought of it, watching for the sake of learning, without having to endure the pain of lived experience. I tried to rationalize with myself. ‘Relax,’ Deep Breath. ‘You’re only a student. You’re just here to learn.’
At the time, my preceptor and I walked into the patient room together and greeted him with smiles and brightly asked him how his day was going. This time it felt wrong. There was a sucker punch coming and only we knew it.
Shortly after the niceties, my preceptor sat down at the patient level, took a breath, and said with compassion and efficiency, “We’re reviewed the results of your CT. I’m so sorry, but it looks like you have cancer. At this point we don’t know where the cancer started from, but it seems to have metastasized.”
A pause. “Okay” the Mr. Smith responds. His face remained hardened and strong, though there was no one with him for him to be strong for. He waited for us to say more.
“I’ll be referring you to an oncologist,” my preceptor continued. “It’s really important that you go to that appointment as soon as possible. I want to make sure that you aren’t delayed in treatment if that’s what you choose to do.”
I watched as his face changed from blank, to angry, to confused. My preceptor didn’t realize that the news has not yet landed.
“I don’t understand,” he responded. “I quit smoking and I had a full CT less than a year ago! And there was nothing there! Nothing!”
As I watched the scene unfold, I felt a sense of dread wash over me as if I was a small animal backed into a corner. I wanted to leave the room as fast as possible. ‘I shouldn’t be here, I shouldn’t be here.’ I kept thinking. ‘This is private. I shouldn’t just stand here and watch.’
But despite this anxiety, face-to-face with true vulnerability, I was honored to be a witness to medicine at its most human level. I stood quietly as the patriarch in front of me slowly appeared smaller, more honest, and more fragile. True imperfection. In a way, it was beautiful. Pure.
A few weeks after Mr. Smith’s diagnosis, his daughter and I sat together during his first oncology appointment. She told me her husband had recently left her and she was caring for her father and her son on her own. When they called his name for the appointment, she grabbed my hands in hers, looked at me and pleaded, “Please. None of this medical stuff makes sense to me. You understand it. You can help us.”
At the end of the day, I chose medicine. I continue to choose medicine, in the words of philosopher Emmanuel Levinas, “For others, in spite of myself, from myself.” Even when the diagnosis is beyond our control, even when following patients hurts, I choose this field because this is important work, because it needs to be done, and as I continue to learn over and over, it needs to be done with compassion. I did not change Mr. Smith’s prognosis. I did not prolong his life. But I provided a comfort to a family in struggle. I was a strong hand when someone needed strength. And in doing so, I became a part of his journey, and now he is a part of mine. That alone is a gift.

Grace Newell, Class of 2023
As I walk down the hall of the ICU toward your room, I know I am about to encounter something new. Just two days ago...
Read More
Grace Newell, Class of 2023
As I walk down the hall of the ICU toward your room, I know I am about to encounter something new. Just two days ago you were rushed into the hospital with excruciating abdominal pain: a perforated bowel, likely an adverse effect from your chemotherapy for ovarian cancer. Just two days ago you shared your story with me despite your extreme pain. Our conversation did not hide the fear in your eyes; fear of not knowing what would happen after your surgery. I shared your fear, my instincts telling me that what lay on the other side of this surgery was something no one wished for.
“Will she be okay?,” I asked your surgeon anxiously throughout your surgery, “She is only in her forties and has a husband who loves her. I hope she will be okay.”
Even as I said these words, I knew deep down inside that your chances of a long-term survival were grim. In fact, the answers to my questions lay right in front of my eyes as I looked at your pale, lifeless organs that reminded me of something I might see in an anatomy lab and not in the operating room. When we opened your abdomen, tumors throughout your entire peritoneum stared back at us. Your bowel was worse. It was so badly damaged from the chemotherapy that your surgeon described it as “frozen bowel,” unable to move or function due to the toxic medication intended to help you survive.She is only in her forties, she still has a whole life to live, I kept thinking as each minute went by and your chances of survival dwindled even more. She is younger than my mother. It was this thought that would haunt me for days to come.
Your surgeon, and then I, spoke with your dad. “I am so sorry that this has happened. Her surgeon did a good job and took the best care of your daughter that he could. I am here if you need anything, and I will be in every morning to check in on her and on you,” was all I could say.
I had no words to describe my own feelings, as I was still processing them myself. When we left your father, it was 4:00 AM and I could tell his world was flipped upside down. As we walked away to get ready for the next surgery, regret pierced my head. Did I make a mistake? Should I have stayed and sat there with him after the night he just had? But if I did that, would there be anything that I could have said to make this situation better? Frankly, I am not sure what I could or should have done in that situation, but I still think about what I might have done differently.
The next day you were awake and moderately aware of what happened the day before. Now, the fear in your eyes was met with somnolence, anger, and frustration. “How are you feeling?” I asked, even though I was afraid I already knew the answer. You shared your frustration about not knowing what would happen next. You wanted answers, but I did not have them. I felt bad I couldn’t help you in that moment. I knew you were hurting and I knew the reality of your condition was slowly sinking in. There is so much I wish I would have said to comfort you in this time, but I couldn’t find the right words to help. “I will make sure all your questions get answered, and if there is anything else I can do to help please let me know. I am here for you and as a medical student it is my job to be an advocate for you,” I explained. Then I left your room not knowing that was the last thing I would say to you before you were sedated, intubated, and transferred to the ICU.
It all happened so quickly. One day I was talking to you and you were responding. The next thing I know I was standing next to you and I was still talking, but you couldn’t respond. It felt unusual for me to talk to someone whom I knew would not respond, but it felt necessary. “Good morning,” I would begin, “It’s Grace the medical student, and I am here to check in to see how you are doing.” Clearly she is not doing well, I would think to myself. However, I continued, “I am going to perform a physical exam and I will walk you through what I am doing.” I listened to your heart and lungs. I examined your dressing that was covering the opening to your abdomen that was never closed. I looked at your ileostomy and documented my findings. At this moment I became haunted again by my recurrent thought: She is younger than my mother. Then, I looked at your face where I once saw fear, anger, and frustration, but now saw peace and tranquility. I held your hand and said out loud, “It was nice seeing you again this morning, I will see you again tomorrow.”
I looked at your father, who responded, “Thank you for coming to see her today. I am glad she is no longer in pain.” I let him know I was here if he needed anything and the nurses were just outside the door. I left your room, just two days after meeting you thinking to myself, I hope to see her again tomorrow.
The next morning you were gone. You passed quietly in your sleep with your father right next to you the entire time. You were younger than my mother, you still had so much life to live, and I continue to wonder if there was something more I could have said to comfort you in your last days. It is funny how much communication can change in just a few days. One day you and I were able to have a conversation, and the next day I find myself talking to someone who I knew was never going to talk back.
_______________________________________________________________________
**Photograph taken by author, Grace Newell, with a black and white film camera then developed in a darkroom.
“To me the leaf reminds me of what we saw during her surgery. Something fragile and lifeless, yet something that was so beautiful that was part of something bigger than the damaged spots that lay on the dying leaf. Just like the tumors taking over her body when her beauty and strength overpowered what she was battling with.”
Arsalan Ali, Class of 2024 and Benjamin Jacobs, Class of 2024
Arsalan Ali “I feel very alone.” After several months of being completely online for medical school due to the pandemic, my life started to feel...
Read More
Arsalan Ali, Class of 2024 and Benjamin Jacobs, Class of 2024
Arsalan Ali
“I feel very alone.”
After several months of being completely online for medical school due to the pandemic, my life started to feel like a never-ending loop within my one-bedroom apartment. Wake up at the same time, turn on my computer, attend class from a small box, eat lunch, study at the same desk for another few hours, eat dinner, and repeat.
The days of the week began to blur together and the boundary between school and home collapsed. I was on autopilot, and I was just going through each day feeling dissociated from my own body, mind, and emotions. I put on a fake smile around others and hoped they would not intuit how I really felt; alone, trapped, defeated, and frustrated. I created a facade subconsciously to show others that I have what it takes to be in medical school, and I am not easily broken. As a first-generation student, I realized at an early age I have to be grateful for the opportunities presented to me. I have never felt empowered to the right to complain as my parents have sacrificed so much for me to be here. Growing up, my dad continuously reinforced to me, “get an education so that you don’t have to work as hard as me.” My dad was the son of a farmer in India. It was deemed that his future would also make him a farmer, but my dad hoped for a future where he could provide his children with a proper education. When the opportunity came to come to America, my dad seized the chance. He came with no education beyond middle school and little to no English.
For over 15 years, my dad worked multiple jobs at the same time, but his mind was just focused on his children to get an education. Despite our financial situation, my parents ensured that I had school supplies and access to tutoring if needed. As I would moan and groan about school, he constantly insisted that education is the key to a better life. Soon enough, his constant reminders and motivation kept me focused on school and to always try my best under any circumstances. Although my background has helped me get far in life, ironically, it was my biggest pitfall during the pandemic.
When I was accepted a position at TCU and UNTHSC School of Medicine in May 2020, it was a dream come true. The years of studying and countless hours spent on MCAT preparation were finally going to be worth it. Like many students starting a new chapter of their life, I could not help but daydream about medical school. I was excited and anxious to move away from my hometown for the first time and meet my classmates. I heard from many mentors that although medical school is challenging, it was the best time of their lives. It was a place where they felt challenged every day and met their lifelong friends. I know now that it was naive to have this “perfect” vision during COVID-19. I was overly optimistic that the pandemic will vanish by the time I started school in July. November: “The cases are still rising and we are unsure when we will be back in person,” said the official message from the school of medicine. At this point, the zoom fatigue was in full effect, and I was a prisoner in my own apartment. Confined to a small space, making laps around the kitchen counter to stretch my legs, and feeling more alone as time passed. I am an avid believer that you learn medicine in a community, and in a virtual world it becomes easy to dissociate yourself with just a click of a button. I was timid to share this feeling with the rest of my classmates as I did not have a close bond with many of them.
It was not until our school did a class survey which revealed that on average our class does not feel connected to each other, however, 65% of us “extremely” wanted to make this connection. For the first time, I felt like I was not alone, but in fact there were nearly 60 other students who felt just like me. As we began to have more in person interactions, our class bonded over this similar feeling. We all wanted to feel a sense of belonging and develop deep connections. After a year of being restricted to a small video square, our class is finally getting the opportunity to finish our phase 1 curriculum in person. It almost seems surreal that after months I am going to get a glimpse of that “perfect” vision of medical school. The year was relentless, and I had to be the same. It was a ‘year of missing’ in medical school- missing traditions and making memories, missing home, missing the feeling of being surrounded by your classmates, and missing the feeling of wellbeing and joy. All of these are important for student life balance, and as I reflect on this year, I have grown so much as a person and a student. The pandemic has shown me that loneliness is real and human connection is crucial for wellbeing. I am ready to continue being relentless and grateful for everything that comes my way as I begin my second year of medical school with the #strong60.
Benjamin Jacobs
Resilience is defined as “the capacity to recover quickly from difficulties; toughness.”
All my life I had to be resilient. When I was growing up, my family moved constantly– so much so that by the time I graduated high school, I had attended eight different schools in multiple states. The longest run I ever had in a single school growing up was three years. The hardest part about being the “new kid” all the time was making friends. Making friends was exhausting because I felt like I was intruding on friend groups that had been formed for years. In the back of my mind, I knew that when I moved to a new school it was only a matter of time before my family would move again. This feeling made me timid and apprehensive to get close to people because I didn’t want to start a friendship, get close to someone, and have to deal with the sadness of leaving them.
When I graduated high school, I knew college would be yet again another test of my resilience. For college, I went to the University of South Dakota (USD) in Vermillion- a small town of 10,000. The four years I spent in Vermillion was the longest consecutive amount of time I had ever spent in one community. There is something special about being in a small community- everyone leans on each other for support. This connection and consistency was something I had always wanted but never had. My experience at USD made me realize that for medical school, I wanted to go to a program with a small class size-where everyone leaned on one another.
When I received my acceptance call from the TCU and UNTHSC School of Medicine on November 1st, 2019, it was the best day of my life, filled with a rush of conflicting emotions: excitement, fear, anxiety. I knew that medical school would be a big transition and perhaps the biggest test of my resilience yet. When the COVID-19 pandemic began shutting everything down in March 2020, I remained optimistic: “Surely everything will be under control by the time I start medical school in July…Right?”
Flash forward: a majority of my first year of medical school was completed remotely from my 15-inch laptop screen at my apartment, guided by a small path through my apartment. Every day I would wake up, walk two feet over to my desk, sit there for hours, and when it was time to go to sleep, I would walk two feet to my bed. Rinse and repeat. My routine was identical regardless of the day of the week; the days began to all blend together.
When my friends and family would ask how medical school was going, I put on a happy face and told them it was going great. I exaggerated how much my classmates and I were interacting despite the pandemic and downright lied at times about our classes being in person. Why? I think this facade I was putting up to my family and friends served as a coping mechanism for me. I would tell them about how my classmates and I went exploring the town (when we really just talked in the parking lot) or how clinical skills in person was nerve-wracking but exciting (when it was actually online). I was living vicariously through the stories I was telling my family and friends.
Being remote made me realize how much I craved physical touch. Something as trivial as a hug, handshake, or even a fist bump between two people just feels human– this was one element that made me feel so disconnected and alone over the past year. Even when we did have class in person and I was finally able to put my hands on a patient, we each had masks, goggles, gloves, and face shields. It felt forced and artificial. Ironically, I realized at some point that the closest I got to putting my hands on a patient my first year were the dozens of prostate exams I was taught to give by my preceptor in clinic. How odd is it that I couldn’t shake a patient’s hand, but had to perform an invasive exam like this one…
But, I wasn’t alone in this feeling. In the clips of speaking with my classmates six feet apart in parking lots or in masks or through screens, we all felt this irony: that some of our most consistent forms of touch have been through our training to perform some invasive and uncomfortable exams on patients.
This past year was not easy, but it taught me that whatever situation you are going through, no matter how difficult it may seem, someone else is going through it too. That is what unites us.

Toni Igbokidi, Class of 2024
Inside rooms where spirit is tethered to time Lie incubators — warm and full of gab, frisk with Glimmer and giddy — defiant souls of...
Read More
Toni Igbokidi, Class of 2024
Inside rooms where spirit is tethered to time Lie incubators — warm and full of gab, frisk with Glimmer and giddy — defiant souls of lesser green grass Naive whetted scalpels and abandoned bellies Naive to Caesarean sutures, iron-bounded one too few Naive of dread towards strange fruit and hooded men — white She stands tall in the wilderness of trees born steel and nitrile stockings Majestic like high-jumping gazelles, where no heights are Greater than post-partum hypertension or gestational diabetes Her father tells her that she is Brown Sugar in a white coat And that her smile creates Rainbows out of raindrops sphering over horizons obscured Epidurals pierce through spine colored with Melanin and scar tissue left by ancestral lashes Nourishment — discovered amongst the juxtaposition of her mother’s tears and prayers Outgrowths of bantu knots and unwavering resolve Reveal that she is standing on the precipice of her own presence Giving birth to a new era of woman

Juhi Shah, Class of 2023
In the webcomic The Oatmeal, illustrator Matthew Inman tackles the backfire effect. He goes on to discuss how the part of one's brain called amygdala "makes...
Read More
Juhi Shah, Class of 2023
In the webcomic The Oatmeal, illustrator Matthew Inman tackles the backfire effect. He goes on to discuss how the part of one’s brain called amygdala “makes us biologically wired to react to threatening information the same way we’d react to being attacked by a predator.”1 Inman’s comic was a popular statement in anticipation for the 2016 election and presently remains relevant due to its wry humor and ongoing significance on why people are so resistant to hearing contradictory facts. However, many political scientists found it hard to replicate as a large-scale peer-reviewed study could not reproduce the findings.2 I felt myself backfiring from reading the backfire effect. This phenomenon is the epitome of how debates begin, of how medical ethics are handled, of how scientific research is initiated.
The motivated reasoning and confirmation bias that Inman discusses in the backfire effect can be manipulated in medicine, similar to the “truthiness” model. Dr. Jeffrey Matthew from the University of Wisconsin adopts Stephen Colbert’s illustration of the “truthiness” model as “Truth that comes from the gut, not the book.”3 The backfire effect and the “truthiness” model are some of the reasons as to why trusting the knowledge that professors, peers, or anyone else impart is so difficult for me. From one angle, I could see the controversial information that was taught to me as something that is just testing the resistance in my amygdala.
I observed the bleak reality of clinical based medicine as something that has been anecdotally passed down to form “truthiness” yet have no evidence-based methodology. For example, we were taught the five most common causes of postoperative fever with one of the causes being atelectasis (partial or complete collapse of lung). However, the relationship between atelectasis and postoperative fever is unsupported. This ongoing tug-of-war between what is factual and what is practiced is the foundation of curiosity in medicine. It’s why I was interested in this profession in the first place.
I was looking for answers. I did not want to look for them in books. That is why I consider our clinical rotations, known as the Longitudinal Integrated Clerkship (LIC) a perfect program for students like myself. TCU & UNTHSC School of Medicine’s LIC incorporates multiple specialties in one longitudinal rotation for approximately 40 weeks. This type of integrated learning allows us to test controversial information such as indication for which diabetes medication to prescribe in the various specialties. These experiences allow us to decide upon our self if these “clinical pearls” are a part of the backfire phenomenon or a form of “truthiness”.
Several patients one day presented with evidence-based urgency hypertension, something I had recently read about but had not yet seen in my patients. These patients had blood pressures well over 180/100 such as 191/106 and 185/103, whereas normal blood pressure is 140/90. Proper protocol from my notes would suggest “oral antihypertensive agents, including β-blockers, angiotensin-converting-enzyme (ACE) inhibitors, or calcium channel blockers.”4 Proper protocol in my clinic: perform the HPI for the patients concerns and not address the hypertension. Talk about backfire.
I began to question if evidence-based medicine is preferential over clinical based medicine. I asked my internal medicine preceptor her thoughts on the difference between clinical based and evidence-based medicine in this scenario and she stated “What evidence-based medication does not always take into consideration are the social factors such as patient compliance and adherence along with socioeconomic disadvantages. When those factors arise, that is when clinical based medicine becomes preferential to evidence-based medicine.
This is where I had to start learning the difference between clinical based practice and academic based practice. I found several articles on UpToDate that both supported and contradicted the clinical based practice in measuring high blood pressure in the clinic. My realization from this search was exactly what Dr. Jeffrey Matthews touched on in his lecture: “evidence is elusive.” Proper protocol depends on what year of research does the physician base their protocol on, the type of medicine (clinical or evidence-based) the physician practices, and just the physician her/himself. Now that I have learned, seen, and practiced the difference, this is a lesson that will never be forgotten.
By any circumstance, this narrative piece is not me passing judgement. This reflection is about me ultimately realizing how medicine is fluid with waves of preference in evidence-based medicine or clinical based medicine. As a naïve medical student, I supposed the two would be one. Oh, understanding that the two types of medicine are rarely unified backfired on me- and my amygdala, the emotional cortex that hosts our core beliefs!
1 Inman, Matthew. “You’Re Not Going to Believe What I’m about to Tell You .” Comic strip. The Oatmeal, 2016. https://theoatmeal.com/comics/believe.
2 Haglin, Kathryn. “The Limitations of the Backfire Effect.” Research & Politics 4, no. 3 (2017): 205316801771654. https://doi.org/10.1177/2053168017716547.
3 Truth and Truthiness in Surgery . Truth and Truthiness in Surgery , 2016. https://youtu.be/swYKy_u3If0.
4 “Emergent Hypertension.” USMLE-Rx. Accessed June 2, 2021. https://usmle-rx.scholarrx.com/rx-bricks/brick/CP_CAR0087.

Lauren Moore, Class of 2024
I named you “Babar.” A familiar fixture on my face so permanent Bloodied blisters bloomed where skin and plastic met. The soft space between lip and nose wrinkled from weeks...
Read More
Lauren Moore, Class of 2024
I named you “Babar.” A familiar fixture on my face so permanent Bloodied blisters bloomed where skin and plastic met. The soft space between lip and nose wrinkled from weeks of crusted snot and Surgical tape. Our initial introduction was a bitter omen For the month that lay ahead. And I, a nonconsenting participant, fought wildly Against the pain while attempts to unify us failed— Repeatedly. One Two, three, Four, five tries before soothing voices whispered “swallow.” You were there stroking my gag reflex as Blood and tears leaked down my sweat-stained face. Just you and me, Babar. My parents fled the room To escape the attack on my nasal cavity. But they would come to know you too. Our union, My elephant appendage, would be the center of the circus And a brazen burden on all. For weeks noxious green flowed freely through you— A fast track from stomach to the external world. Internal physiology exhibited for all to gawk, an intimate connection Requiring diligent hands to sustain filling demands. Clamp, empty, connect, repeat. I pleaded for water while you sucked me dry. An assault of daily depravity and cruel balance of power yet— I grew to love you. Together we weathered Surgeries, sepsis, starvation. 20 pounds we lost together Catheters, a central line, and drains. A comradery visible yet unfelt among observers For you both delivered and understood my pain. But then ice chips replaced cracked lips As food for blood was swapped for solids, And I was left abandoned in your wake. Freedom was redefined by your depleting grasp And I forgot how to receive. I dreamt of liberation, but fullness led to rejection. Offerings of cotton candy ice cream, confetti sprinkles, And stinging bile swirled in a bedpan. Days spent begging for relief replaced with hopes of emptiness— A mouthwatering sickness of conflicting desires. Was it the gift of life or hefty price for outsmarting death? A searing throat from eating then retching. Retching then eating. Fond memories of us now fleeting.

Dilan S. Shah, Class of 2023
She was my first real patient. Before the pandemic, I regularly saw her at my family medicine clerkship for routine follow-ups. Always accompanied by her...
Read More
Dilan S. Shah, Class of 2023
She was my first real patient. Before the pandemic, I regularly saw her at my family medicine clerkship for routine follow-ups. Always accompanied by her adoring daughter and designated caretaker, they would teasingly call me “baby-doc” as I fumbled with my stethoscope.
Now, almost a year later, I was holding her small bowel between my gloved fingers under the bright lights of the OR. As I ran my hand down the loops of intestine, I felt crunching– “I think I feel pneumatosis intestinalis,” I said to the surgeon. He met my hand at its place on her bowel and felt. “The kid is good,” he said to the scrub nurse, “nice catch!” Oh the validation of a correct diagnosis. Though eager excitement quickly made way for dread. I knew what this meant. Her intestines were dying, she was at the end of the road.
We met again 7 days ago in the emergency room when I was on-call. Fear of coming to a hospital full of COVID left her in agony for months as she ignored early signs of her dying organs. Serendipity or fate, when she did finally come for help, I was there.
I was with her in the hospital room, where she laid helpless, vulnerable and scared. I was with her in the OR where she laid open, vulnerable and exposed. Balancing the duality of humanity and science, I held her daughter’s hand after each surgery and translated the surgeon’s medical jargon. I was the last person she talked to, giving soothing words as the anesthesiologist put her under, never to awaken again.
Her final days were spent unconscious and intubated in the ICU. Her daughter was by her side every day, for as many hours as COVID policy allowed. Between patients, I would go down and visit them. We would sit and I would listen to her daughter tell stories of her kind and quick-witted mother.
On the final day of my Surgery rotation, and what I would later discover would be her final day of life, I wrote her family a letter. Simply to share how grateful I was to have learned from their mother’s case, wishing them peace in the soon-to-be passing, and offering whatever soliloquy of comfort I could. It was a simple gesture, one that I figured would be met with a few moments of gratitude and then slip to the back of their consciousness and forgotten in grief. Months later, her daughter would reach out to me to share how impactful that simple gesture was for her family’s coping.
I chose medicine, because in no other field are you stretched to be both so technically proficient and emotionally vulnerable. The science of medicine is constantly infused with the raw emotion and heavy responsibility of having a human life in your hands. To have such privilege is a beautiful burden.

Caden D. Duffy, Class of 2024
I walked into the patient’s room and saw my sister. At least, Mary* could have been my sister for her age and complexion seemed to...
Read More
Caden D. Duffy, Class of 2024
I walked into the patient’s room and saw my sister. At least, Mary* could have been my sister for her age and complexion seemed to match. As I opened my mouth to speak, her shaking hands, thick palpable nervousness, and a downwards stare portrayed an individual uncomfortable and unaccustomed to a physician’s office. I greeted her with a smile, stating my name, position, and purpose. Just as I had with the patients before her, my first question was to ask why she had come in. The words—“I’ve been feeling depressed”—were quickly and quietly spoken.
I witnessed Mary’s familiar face lower to the floor as her quiet, delicate nature came to light. I felt a reverence for her feelings of grief, a scene that might quickly be compromised due to my inexperience. It took a few moments, but she gradually warmed up to our discussion as I centered the interview around her journey to the office. We talked about her mother’s supportive and guiding influence which had led her to request the visit. We discussed the coping mechanisms she was trying, including an increased reliance on marijuana, which had proven unsuccessful in warding off feelings of self-doubt. I reassured her that the attending physician would provide excellent care, good enough that I would recommend him to my own sister. A vivid image of my sister passed through my mind. I could see her, or them. My conversation with Mary felt familiar.
Despite that I had never worked with a patient challenged by mental health concerns, my confidence in understanding Mary climbed as I completed her interview. Perhaps due to her semblance to my sister, I left the room with what I felt to be a complete picture of her condition. As I began my oral presentation to my preceptor, I boldly told him of her one-year history of feeling depressed. I described in detail her symptoms, including nausea and vomiting, which I proudly deduced had stemmed from her use of marijuana.
The seasoned physician listened patiently and then paused for a moment. “Did you ask Mary if she’s ever considered killing herself?” he asked. I stared back at him. I was tempted to try and rationalize why I had not, especially with all of the other important history items that I had obtained. “No,” I frankly replied back, somewhat embarrassed by overlooking what he knew was a key part of her history. Like an expanded balloon experiencing an air leak, I felt the common deflation of an overly confident medical student. I discreetly tried to cloak the puncture.
Why hadn’t I asked? Without meaning to, I thought about how my sister would never do something to hurt herself. Even with family, suicidal ideation can be a sensitive subject to address. I didn’t want to intensify my discussion with Mary, especially since she had already extended herself in discussing her drug use. Mary was vulnerable in coming alone to a new provider visit. I would need appropriate justification to ask a question like that. If she did struggle with suicidal thoughts, what would I have to do with that knowledge?
As I contemplated these questions, the attending told me about selective serotonin reuptake inhibitors, or SSRIs. They are one of the most commonly prescribed antidepressants. Citalopram, or Celexa, works very well to treat patients who are experiencing depression. However, there is an FDA black box warning prominently displayed on the side of the medication. This warns of the possible increase in suicidal thoughts or actions in some young adults at the initiation of treatment. For these patients, prior suicidal ideation is further investigated with extreme precaution prior to prescribing the medication. If these thoughts are already present, alternatives are further considered. Completely unaware, I had left Mary’s room without a vitally important aspect of her history. Although the medication could improve how she was feeling, giving Mary this antidepressant could contribute to a negative and permanent change to her life.
We returned to Mary’s room and learned that my preceptor’s inquiry was especially important in our visit. I observed the connection that he made with Mary, gathering key information and using her responses to create a treatment plan. We discussed our options and decided to prescribe Mary a different medication. Although the conversation was difficult and personal for Mary, my preceptor’s kind but direct questioning inspired me to better obtain a more complete medical history out of each of my patients.
Someday I may encounter a sister, brother, friend or neighbor sitting in the corner of my examination room. In spite of the familiarity, I need to work towards gaining an unbiased and more complete understanding of the information which could impact their health. Like with Mary, I look forward to understanding who my future patients are, and how best to treat them, through asking the right questions. This will probably not be the last time I walk into a room, and see my sister.
*The patient’s name has been changed to ensure privacy.
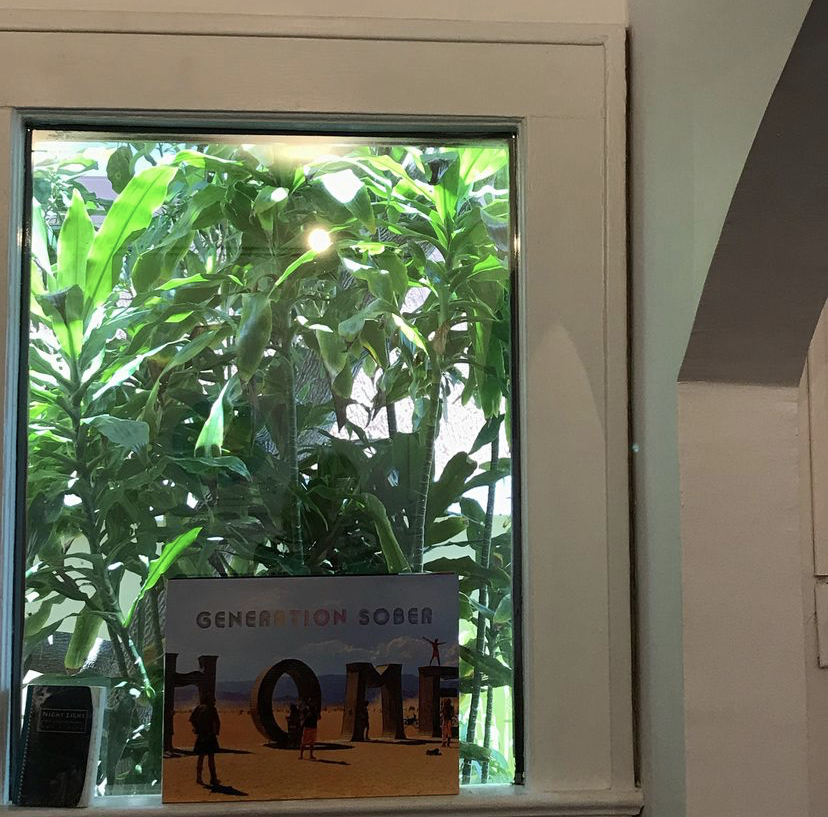
by Emma DiFiore, Class of 2024
Maybe it is the fact that the clinic I have been placed in as a first-year medical student is primarily patients aged 65 and up,...
Read More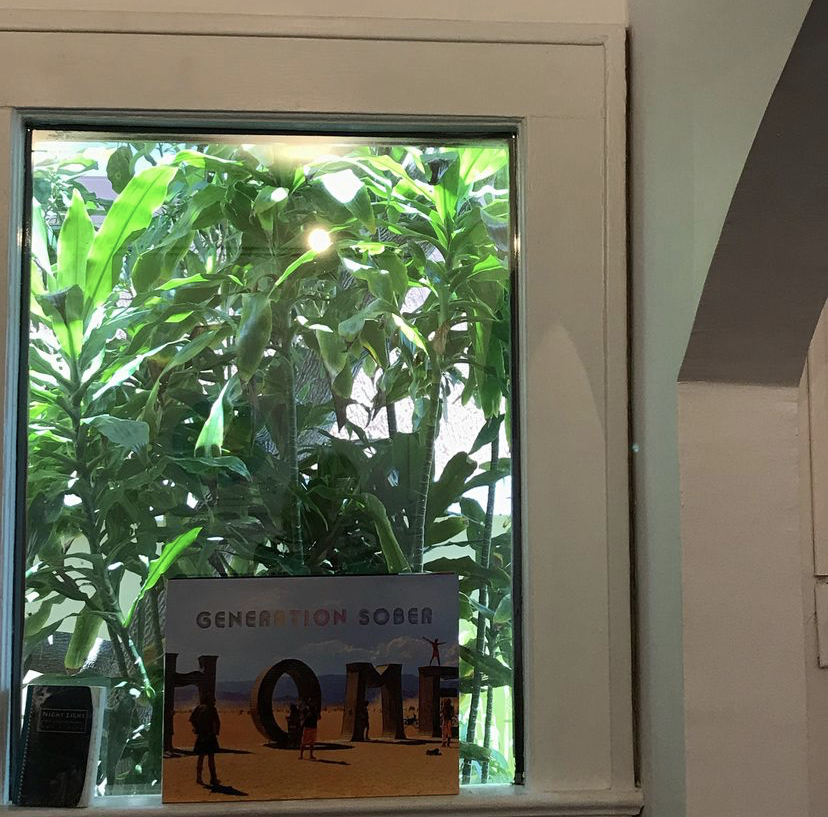
by Emma DiFiore, Class of 2024
Maybe it is the fact that the clinic I have been placed in as a first-year medical student is primarily patients aged 65 and up, or maybe it is the tremendous amount of death we have all faced this year amidst the COVID-19 pandemic, but lately I’ve been pondering what it means to experience death in the field of medicine.
Recently, I had a discussion about death with my clinical skills preceptor, Dr. Ashley Huddleston. She started her career in emergency medicine, constantly in the face of death. She oftentimes only knew these patients as “ill” or “dying” as opposed to in primary care, where patients are seen in all facets of life. Dr. Huddleston has since changed fields of medicine to wound care and hyperbaric medicine: rehabilitation. Now, she gets to watch as her patients experience life. She gets to form relationships with them, often seeing them weekly. Yet, interestingly, she stated that this now makes death more difficult to swallow when it does come. These long-term relationships in outpatient medical care become so pronounced, as opposed to the sometimes unfamiliar nature of relationships in inpatient care. These humans are no longer strangers, but companions.
I cannot predict how I will face death as a medical professional or even as a human. But I do know I want it to be as intimate and raw as the day I had first experienced a healthcare-related loss. I was interning at an outpatient addiction treatment center that summer. It was unexpected. It was angering. It was reality. Here is an excerpt of my writing based on that day:
“A typical Monday morning as an intern at an intensive outpatient addiction treatment center is brimming with positive energy and new beginnings. Pulling up to the office, I would see the clients chatting and laughing on the front porch. Their communal cigarette smoke mingled with the sweet scent of gardenias in the summer air. Inside the center, which resembles a quaint pink cottage, the therapist, the medical director, and a pot of freshly brewed coffee would joyfully greet me. Monday mornings felt like sobriety was at our clients’ fingertips – until it wasn’t.
On July 5th, Monday morning felt dark. The porch was empty and humorless. Its usual inhabitants sat confused and quiet inside the group therapy room. The staff’s office doors remained shut. No one there to greet me. No freshly brewed coffee. Minutes felt like hours as we waited. Eyes scanned the room to see who was there and who was not. With heads bowed, the staff entered and took their seats. The silence was finally broken: ‘Joe; had overdosed and passed away. Joe, the one who everyone in the program looked up to, who was thought to be the last person this would happen to. Addiction had won, and its triumph rang loud in the silence of the room.
I have regularly come back to that somber July Fifth when Joe lost his fight. That day,
there was a sense of quiet perseverance. Reflecting back, I realize how difficult it was to retain such fortitude amidst tragedy. Nonetheless, each one of us left holding our heads a little higher — the patients, the therapists, the physicians, and me. The patients persisted in their fight for sobriety. The therapists and physicians persisted in their inclination to treat those suffering. I, aching for that same inclination, persisted in my pursuit of medicine. In that vulnerable moment, gripping each other’s shaking hands and wiping our weeping eyes, we were able to bridge the gap between patient, intern, and provider. There was a genuine camaraderie that day which left us all at ease.”
This memory is frozen solid within me. And it was what pushed me closer to medicine. In fact, without this experience, as tragic as it was, I do not believe I would be where I am today. It is not that it motivated me, it is that it matured me. It revealed to me the realities of medicine, while erasing the previously glorified view I had of medicine as simply healing.
Will this experience prepare me for future confrontations with death? Possibly. I just hope whenever death comes, I am surrounded by people in the most humanely raw way possible. No hierarchical labels of physician, resident, student, or patient — just fresh human emotions, compassion, and perseverance.

Do you have a HuMed inspired photography series you'd like to submit? Visit our submission page to send us your ideas or connect with Erin...
View PhotosDo you have a HuMed inspired photography series you’d like to submit? Visit our submission page to send us your ideas or connect with Erin Nelson, PsyD to discuss.
Prisca Mbonu, Class of 2026
The first step into the Cold cadaveric laboratory The first whiff of formaldehyde That seems to permeate the walls The first moment when the shiny...
Read More
Prisca Mbonu, Class of 2026
The first step into the
Cold cadaveric laboratory
The first whiff of formaldehyde
That seems to permeate the walls
The first moment when the shiny zipper is pulled
To reveal what is hidden beneath
The first cut through skin
Into fat, fascia, and finally, muscle
The first surge of guilt
At the sacrifice of another
The first feeling of gratitude
Towards a complete stranger
There lies a place card
Mounted against a rusting metallic stand
With words printed on a purple, laminated sheet
They tell me what is left of you
Age. Sex. Cause of death.
But your body tells an even greater story
Of pain, surgical scars
Of adventures, tattoos
Of joy, laugh lines
Of hard work, calluses
Of life, childbirth
In you, I see a collection of firsts too
Ngoc Bao Nhi “Mariana” Nguyen, Class of 2027
Part A (Brief description of chief complaint): Iron Deficiency Anemia: Iron is essential in making hemoglobin, a protein in red blood cells. Iron deficiency anemia...
Read More
Ngoc Bao Nhi “Mariana” Nguyen, Class of 2027
Part A (Brief description of chief complaint):
Iron Deficiency Anemia: Iron is essential in making hemoglobin, a protein in red blood cells. Iron deficiency anemia is a condition in which blood lacks adequate healthy red blood cells due to low level of iron. Common symptoms include fatigue, irregular heartbeat, pale or yellowish skin, and cold hands.
Part B (Poem):
I lack red blood cells
Lightheaded, sometimes I get
I need grass-fed beef.

Ngoc Bao Nhi “Mariana” Nguyen, Class of 2027
Part A (Brief description of chief complaint): Iron Deficiency Anemia: Iron is essential in making hemoglobin, a protein in red blood cells. Iron deficiency anemia...
Read More
Ngoc Bao Nhi “Mariana” Nguyen, Class of 2027
Part A (Brief description of chief complaint):
Iron Deficiency Anemia: Iron is essential in making hemoglobin, a protein in red blood cells. Iron deficiency anemia is a condition in which blood lacks adequate healthy red blood cells due to low level of iron. Common symptoms include fatigue, irregular heartbeat, pale or yellowish skin, and cold hands.
Part B (Poem):
When the iron is running low,
A shadow of fatigue begins to grow.
Pale echoes in each step I take,
Anemia’s weight, a heavy ache.
In veins, a river without its might,
Transferrin, the captain, lost in the night.
Cells, like soldiers, weary and dried,
Battling fatigue, a crimson tide.
When the iron is running low,
Hematocrit staggers below.
Heart’s rhythm stumbles in faltering beat,
A symphony of exhaustion, a silent defeat.
Blood cells fade in ghostly wail,
In the mirror, my complexion pale.
Cold fingertips where blood don’t flow,
When the iron is running low.
A labored sigh in every breath,
Iron’s death, my own Macbeth.
The world spins, a dizzying show,
When the iron is running low.
Iron returns in distant dreams,
In languor’s grip, a silent scream.
Yet hope lingers like a resilient ember,
For iron’s return, a strength to remember.

Ngoc Bao Nhi “Mariana” Nguyen, Class of 2027
Part A (Brief description of chief complaint): A cold is a common viral infection of the nose and throat. Symptoms include runny nose, sneezing, and...
Read More
Ngoc Bao Nhi “Mariana” Nguyen, Class of 2027
Part A (Brief description of chief complaint):
A cold is a common viral infection of the nose and throat. Symptoms include runny nose, sneezing, and congestion. Because antibiotics only fight bacteria, and not viruses, they’re usually ineffective against colds. The condition is usually harmless and mostly resolves on its own within two weeks.
Part B (Poem):
With sniffles and sneezes, he caught a cold,
In bed he rested, his sinus consoled.
No pills would he take,
Just warm tea with cake,
A viral invasion, not bacteria, behold!
Naimah Sarwar, Class of 2025
And he beams, I’m golden, just golden. I’m golden and also, what exactly is a seizure? You see, he’s been drinking that Golden liquid, his...
Read More
Naimah Sarwar, Class of 2025
And he beams,
I’m golden, just golden.
I’m golden and also,
what exactly is a seizure?
You see, he’s been drinking that
Golden liquid, his golden ticket
home. His ticket back to
his golden days, a golden daze.
That heart of gold irradiating
his skin.
Will you think about quitting?
A crescent moon, ear to ear.
I’m golden,
everything is golden.
Golden boy
his eyes, all that glitter.
Jayesh Sharma, Class of 2027
Part A (Brief description of chief complaint): Migraine with aura is a type of migraine headache characterized by the presence of sensory disturbances, known as...
Read More
Jayesh Sharma, Class of 2027
Part A (Brief description of chief complaint):
Migraine with aura is a type of migraine headache characterized by the presence of sensory disturbances, known as an “aura,” preceding or accompanying the headache. The aura typically involves temporary, reversible visual, sensory, or language disturbances that develop gradually over several minutes and usually last for less than an hour.
Part B (Poem):
My eyes open to stark cacophony
Sharpened colors,
Cutting me with their keen vibrancy
Jagged sounds,
As if hitched breaths
Hiding from nearby pursuit
I blink rapidly
Trying to find my place;
A lone straggler
Moored on a lost island
A cloud passes
Rolling past brief farewells
Frosted pearls
Flooding into a conductor’s crescendo
A neighbor glances
Assuming narcissistic attention
Brief windows opening
Caught under heavy fantasy
A babe wails
Fighting confusion with volume
A solo instrument
Caught between fractured arpeggio
I try to stay afloat
flailing with a fool’s futility
Assuming survival
to be adequate reprieve
These blurred lines adjust
as grief tends to do
Moving from pounding beats
unto dull aches
Dragging marionette limbs
Into rehearsed movement
The moment passes
Or perhaps I tell myself it does
Swaying to faint decrescendo
Distraction replacing reality
An easy pivot,
One I have grown accustomed to
Both eyes close once more
Doorways bleeding light
from what they hide behind;
A hopeful illumination
A slight knocking,
as if not to startle beauty awake
I relish my brief ignorance
Into the dread of inevitable beginning
as if sensing a conductor’s crescendo
Building up into a familiar movement
Slowly,
Towards stark cacophony

Jayesh Sharma, Class of 2027
My father bought a ping pong table. It's nothing special. Two sides of green space separated by a thin, rectangular net. Blue and red-halved paddles,...
Read More
Jayesh Sharma, Class of 2027
My father bought a ping pong table.
It’s nothing special. Two sides of green space separated by a thin, rectangular net. Blue and red-halved paddles, built to accentuate each “tick” and “tock” between opposing sides.
He always asks me when I want to play. It’s as if he wants to justify the hassle of getting this table by using it as much as we can. He was the same about his pizza maker, camera, and lawnmower. He’s a dad in normal ways like that, finding color to tint dull days.
Playing with him is quiet.
“Tick.”
“Tock.”
“Tick.”
“Tock.”
“Ti- ah, close.”
At times, between hits, a conversation will ripple between us. It’ll be something small; maybe mom’s latest gripes, Shruti’s upcoming dance performance, or pieces of wisdom he likes to impart.”
Mostly though, it’s quiet.
“Tick.”
“Tock.”
“Tick.”
“Tock.”
“Ti- ah, I’ll get it.”
It’s a steady beat, one I feel my thoughts playing cadence to. It’s calming, letting me flow as my paddle does.
He spent the first five minutes of our time today adjusting things in our garage. He then felt finicky about how centered the table was, and then about how many balls he could hold. Growing up, these tendencies of his would’ve annoyed me to no end; I would’ve felt that he was wasting time while I just wanted to play. That old feeling hinted upwards still, but now I see things a bit more from his perspective. I realize that he was expressing how he wanted our time together to go smoothly, adjusting small things as his way to protect our time.
I haven’t always liked my dad. I used to feel he was the epitome of who I didn’t want to be. I would then feel frustrated that I still admired him for his intellect and work ethic. We used to argue a lot, especially after my sister was born. Everything, from my independence to his anger, was constantly put on the table with no reprieve. Small times like these, ones where we can quietly enjoy each other’s company across the table, show how far we have come.
“Tick.”
“Tock.”
“Tick.”
“Tock.”
“Tick.”
“To-I have another one, leave it.”
I haven’t always been the best son. But he’s been okay with that. In spaces where our conversations ripple, he’s understood the storm which has come before. We’ve both had irrational times with each other, but we always knew that we would always be in each other’s lives. Sometimes, that fact annoyed me more than anything else.
“Tick.”
“Tock.”
“Tick.”
“To- there we go. Last one?”
“Sure, I’m losing breath anyways.”
Two sides of green space separated by a thin, rectangular net. Blue and red-halved paddles, built to accentuate each “tick” and “tock” between opposing sides. That’s how I used to feel with him. Growing up has allowed me to see that it isn’t that way. At some point, we put down the paddles and walked away together. The ripples calmed, the storm passing.
“Tick.”
“Tock.”
“Tick.”
“Tock.”
“Tick.”
“Tick.”
“Tock.”
“Tick. I technically cheated on the last one.”
“Tock.”
“Tick. Ah well, who’s keeping score anyways.”
“Tock.”
“Tick.”
“Tock.”
…
“Want to play again tomorrow?”
“Sure dad.”

Prisca Mbonu, Class of 2026
We entered the procedure room to find the final patient of the day, Ms. K, sitting upright on the examination table. She had already changed...
Read More
Prisca Mbonu, Class of 2026
We entered the procedure room to find the final patient of the day, Ms. K, sitting upright on the examination table. She had already changed out of her own clothes and into the customary light blue patient gown, with a white sheet draped over her legs. Her manicured hands were clasped together, fingers wringing with uncertainty. “Hello, Ms. K,” my preceptor, Dr. L, greeted. “I have a medical student with me today. Are you comfortable with her observing your procedure?” Ms. K’s gaze shifted towards me, and after a moment of hesitation, she nodded slowly and said, “Sure. The more the merrier, I guess.” After thanking her, I gave my introduction, a routine practiced countless times during my two years of training.
My preceptor handed Ms. K two consent forms which clearly stated the risks and benefits of the procedure. I watched as Ms. K’s barely audible sighs accompanied the turn of each page as she read before eventually signing her consent. Soon after, we were joined by two nurses, bringing the room’s occupancy to a total of five. The procedure we were preparing to perform was an endometrial biopsy. Ms. K, a 58-year-old woman, had been experiencing postmenopausal vaginal bleeding for some time. In such cases, an endometrial biopsy is often an initial test for evaluation.
The procedure involves inserting a device into the uterus to collect samples to help determine the source of bleeding. Understandably, patients often find this procedure to be unpleasant and painful, which contributes to heightened levels of anxiety. Furthermore, the potential outcomes of the procedure only serve to worsen this anxiety. This wasn’t Ms. K’s first experience with the biopsy; she recounted her previous ordeal where inconclusive results left her disheartened and without answers. I understood her frustration at the entire situation, her escalating worry about her troubling symptoms, and her desperate need to finally have a diagnosis.
So did Dr. L, who gently held Ms. K’s hand and assured her that, while some discomfort was inevitable, she would do her best to minimize it. The reassurance brought a grateful, tearful nod from Ms. K, and the room’s atmosphere softened. The rest of us chimed in with words of encouragement, and I noticed Ms. K starting to feel more at ease. “Ok. I’m ready,” Ms. K said with a weak smile. While one nurse assisted Ms. K into the lithotomy position, the other organized the required instruments on a stainless steel tray. As the nurse explained the functions of the speculum, tenaculum forceps, Allis clamp, uterine dilators, and suction curette for my learning, I instinctively positioned myself to block Ms. K’s view of the instruments, fearing that seeing them would amplify her anxiety.
As we prepped, we engaged Ms. K in conversation about her background. We learned that she was born in the Caribbean. She spoke wistfully of the beauty of her homeland, painting vivid pictures of breathtaking beaches adorned with rolling waves and caressed by gentle breezes. She reminisced about cerulean skies and distant horizons that beckoned her each morning. Somehow, the conversation veered into light-hearted banter about handsome men from the islands, eliciting hearty laughter from all of us.
Her nostalgia momentarily distracted her from the impending procedure, but she was brought back to the present at the insertion of the speculum to visualize her cervix. She winced, a soft whimper escaping her lips. “Would you like one of us to hold your hand? You can squeeze tight if it hurts,” Dr. L offered. “Just try not to break our medical student’s arm,” a nurse quipped, and more laughter reverberated through the room with Ms. K joining in. In that room, where tension and camaraderie were intertwined with one patient at the heart of it all, I felt a strange sense of kinship among strangers. Once again in my training, I was reminded of how connections could be found in the most unexpected places.
Throughout the procedure, we continued to offer words of encouragement and lighten the mood with jokes. Ms. K kept her eyes tightly shut, breathing shallowly through pursed lips. Occasionally, a faint smile crossed her strained features. I wondered if behind her closed eyelids, she envisioned scenes of deep blue waters and golden sands from her childhood. When the procedure concluded, I bid farewell to Ms. K and made a mental note to follow up on the biopsy results. I hoped they would provide the answers she needed and bring her the relief she deserves.
Kenneth Le, Class of 2027
Part A (Brief description of chief complaint): Mitral stenosis is the narrowing of the mitral valve leading to reduced blood flow between the left atria...
Read More
Kenneth Le, Class of 2027
Part A (Brief description of chief complaint):
Mitral stenosis is the narrowing of the mitral valve leading to reduced blood flow between the left atria and left ventricle. It can lead to complications such as arrhythmia, heart failure, and thromboembolism.
Part B (Poem):
Rheumatic fever
Fused to my friend, I am stuck
Snap then a rumble

Andrew Armstrong, Class of 2027
Part A (Brief description of chief complaint): Psoriasis is a skin disorder affecting individuals with an underlying genetic predisposition who have been exposed to a...
Read More
Andrew Armstrong, Class of 2027
Part A (Brief description of chief complaint):
Psoriasis is a skin disorder affecting individuals with an underlying genetic predisposition who have been exposed to a “triggering event” such as an infection or medication. Psoriasis manifests as a red, scaly, intensely itchy rash that can occur anywhere, but are especially prevalent on the head, elbows and knees. The rash bleeds easily when picked and can even cause other symptoms like pain in the hands and back, as well as finger and toe nail disfiguration.
Part B (Poem):
I itch my arm, I don’t even realize I do it anymore
It bleeds, it usually does
I don’t realize when that happens anymore
I do realize when people stare, that’s harder to get used to
And they never stop, never
I feel like the lepers of biblical times
They were deemed unclean to live among others
I’m deemed unfit to be ignored
So I pick, I bleed, people gawk
Med students analyze
Tired residents check me off their list of “to-dos”
Attendings use me as a teaching point
But they stare too, they all do
And they never stop, never
I get jealous of the other disorders
Things like burns, broken bones, cancer even
At least people know they can’t get cancer from being around people with it
People always wonder if they can get what I have
Then I feel guilty for that thought
At least this won’t kill me
But I would give the anything for it to stop
Jesus healed the leper
If he came and healed me I wouldn’t forget to say thank you
I wonder if he’d stare too

Ope Duyile, Class of 2026
Polycystic Ovarian Syndrome. Cysts on my ovaries? The shock of it all. Reproduction is not until the next block, I don’t know much…yet PCOS The...
Read More
Ope Duyile, Class of 2026
Polycystic Ovarian Syndrome.
Cysts on my ovaries? The shock of it all.
Reproduction is not until the next block, I don’t know much…yet
PCOS
The PA is talking of metformin and birth control
Isn’t that a diabetic medication? Why would I need it?
I’m too scared to ask. It cannot be. Liiiiike, say it ain’t so.
PCOS
My skin is breaking out.
My neck has gotten darker.
The irregular and painful periods.
The insomnia.
The crazy sweet tooth.
My hair has been thinner lately.
My testosterone is elevated.
The rapid weight gain. The struggle with weight loss. My frustrated efforts.
It all makes sense. It is not entirely my fault. I should not have been so hard on myself.
PCOS
I am a medical student on the other side of a scary diagnosis.
I think about all the ways I want my provider to show up.
I wish I had more time to process and ask my questions.
I wish my message on the patient portal was addressed.
I see medicine from a new angle.
I resolve to be a rock when I deliver an unsettling diagnosis.
To avail myself to my patient through the uncertainty and stages of grief.
PCOS
I scour every article PubMed has to offer. C.R.A.P style.
Something about inositol imbalance and insulin resistance. Metformin begins to make sense.
Something about fertility. I want to be able to have children.
With options come power.
I remember that I am still human. This body of mine is frail. I am angry and disappointed
Why me? I have always had a clean health bill.
When did things change and how did I not notice?
Why didn’t this PA tell me more?
Where do I go from here? What is to come?

Mary Howerton, Class of 2024
Your first climb started so young and performed. From so young you had to climb your way out of terrible memories, hard pasts, tough situations....
Read More
Mary Howerton, Class of 2024
Your first climb started so young and performed. From so young you had to climb your way out of terrible memories, hard pasts, tough situations. Rough childhoods or terrible families, military deployments that showed you the worst humanity can be. That first drink was a surprise, an oasis in a desert of misery. For the first time, you had numbness in your life, and you thought it was the perfect solution. Buddies drinking in barracks or in bars. Drinking culture at its prime, giving you permission to get numb.
Was your next climb the ascent? Noticing you drank more than everyone around you? Starting to drink alone, at home? Perhaps you thought no one would notice. Sneaking away from the family you had to find numbness again. You love them, it’s not them you want to hide from. The drinks you have don’t seem to be enough anymore. Higher count, higher proof, higher concentration to attempt the same high as before. For a time, you couldn’t tell which was the stronger drug- alcohol or denial.
You climbed deeper and deeper into addiction at that point. Physical dependence replaces any psychological one you had previously. Baseline levels just to not feel sick, but those levels made you feel bad anyways. Tremors, sweats. Cutting back but you couldn’t. Feeling stuck. The life you have and the life you want separated by the chasm that is withdrawal.
Climbing into darker and darker depths. And then that news. “We have run some tests and we have important news to share with you. You have cirrhosis or scarring of the liver. Based on your symptoms, your liver is failing to do its job. We will do everything we can to keep you as healthy as we can, but we need to start looking at other options”. In that moment the warm blanket of denial is ripped away. Cold reality sets in. The chill on the path you have set for yourself is so lonely and so cold. Regret is bitter. And there a decision had to be made; do you continue the road you were on, or do you choose an entirely different battle?
The road to sobriety was one of the toughest climbs you have ever had. While I might have some clue about what that entailed, only you know the strength it took to change it all.
Perhaps the most complicated part of this route was what lay ahead. Transplant committee meetings. Transplant lists based on scores. Review boards and waiting for a second chance. All the while your body fights every day to keep up. Fatigue setting in, skin and bones. Yellow and sunken eyes. The body a betrayal of the work you put in the last six months to fight for sobriety.
The days are long, but you keep walking. Your steps slow, and you notice yourself stumbling every few feet. Then falling to your knees. You can’t climb anymore, you think. Collapsing down. You can see the ascent, the end. But it is too far away.
I come visit you in the intensive care unit. Your body is failing, and we have hooked up to every machine we could to keep you alive until a donor is available. Intubated and sedated you lie there, holding onto life. I pull out my notes from my white coat, write down the newest numbers on how you are operating. Notes put away. I grab your hand. I plead and pray for a new liver for you. For a second chance at a mended life. We stay like this for a while before I let you rest for what will be the last ascent, the transplant surgery.
You received your second chance at life at 11:56 pm that same day. Keep climbing. You have already come so far.

Kenneth LeCroy, MD
There is an old joke that asks the question, “How do you want to die?” The answer is a quipping one: “I want to die...
Read More
Kenneth LeCroy, MD
There is an old joke that asks the question, “How do you want to die?” The answer is a quipping one: “I want to die like my grandfather, peacefully in his sleep. Not screaming, yelling, and in terror like all his passengers.” A silly joke asking a very important question.
One of the early steps in Stephen Covey’s book 7 Habits of Highly Successful People is to start with the end in mind. He means to begin by visualizing a life goal and then build foundations and processes that help to accomplish that eventuality. Those goals may or may not be achieved, but the eventuality of death will happen to us all. So how do you want to die?
I would like to tell you a great way to die, but before I get there, I have to tell you some stories.
In 1991 my oldest brother David had a dream that essentially pushed our younger brother and me to go on a five-week trip to and through Alaska. We drove to the Canadian border from San Antonio, Texas—and that was just the halfway mark. (We made it work, but this is not how I recommend traveling North.) Our first stop was Skagway, Alaska to do the fairly grueling Chilkoot trail, a 33-mile stretch of the Yukon Gold Rush. The elevation gain is incredible, with up and down sections repeating ad nauseum. We began the three-day trek with 35-pound packs and were out of food by the last day. On our second day, we were concerned about a group camping nearby—three friends, one in their late 70s, the other two in their 80s. We were discussing whether to share our food with them when we heard the distinctive sound of a bottle of wine opening! We later wondered if we should offer to help them at the pass itself…and they beat us to the top. Had we known we would have been asking them for their help throughout the trip as they were clearly living their best lives while ignoring the number of their birthdays.

We had done the trail. A three-day hike that was a great accomplishment in life. We sat in silence among debris and trash from me that had lived and loved and worked so hard and died one hundred years before us. A humbling moment.
Fast forward 10 days from there. We were in Denali National Park where cars are not allowed. Ingress is by yellow school buses to which the animals have acclimated. We had plans to camp for 7 days, so we packed heavy 55-pound packs and rode the bus for five hours before embarking on a flat 7-mile hike to our site.
The moment we strapped on the packs it was vastly different— I still use this illustration with patients about the benefits of losing 20 pounds. We trudged our way through thick high brush, calling out every 20 or 30 seconds “Hey Bear!”; walking up and surprising an Alaskan grizzly is not wise. After a rest break on the first day, we all struggled like crazy to get on our feet again. David in particular struggled, he slipped and found himself on his back with the backpack weighing him down, as helpless as an overturned turtle. Far from being angry, David laughed uproariously, and the three of us laughed continuously for a long time. From time to time over the years, we talk about that trip to Alaska and always include that moment.
Fast forward now to the Christmas of 1998. My family as a rule would gather for at least a weekend around Christmas to celebrate, and this Christmas was no different. I clearly remember my brother David asking me a question that puzzled me at the time. He asked, “You know that feeling you get when you pass out while you’re laughing really hard?“ I told him that I did not know what he was talking about, and I left it at that. A month and a half later on Valentine’s Day, there was another family gathering to celebrate my mother’s and my brother David’s birthdays (his 35th.) I was unable to go but my wife made it. She mentioned that David was experiencing balance issues and she had seen him hit a wall once while walking down a hallway. He assured everyone that he had seen his doctor and had an MRI pending. A few days after returning from that Valentine’s visit he had the MRI results—and an appointment his primary care doctor had scheduled with an oncologist. I was able to go with him to that oncology appointment. I was completely convinced that he had an acoustic neuroma—difficult to treat, but treatable.
David and I went into the appointment room together. It was a small exam room in the Cancer Treatment and Research Center of the University of Texas Health Science Center at San Antonio. Along one wall was a bank of X-ray view boxes and MRIs attached to the wall. Instantly I was disappointed in the center because they had clearly left the previous patients’ MRI up and allowed David and me to enter. I briefly glanced at the X-rays and could see an obvious large tumor…the previous patient was, as our Alabama relatives would say, an absolute dead person. I was approaching the end of my third year of residency in family medicine, and I knew this was a grave patient privacy violation. The physician eventually came in and began to talk to us and to my shock, quickly turned to the x-ray view boxes and directed our attention to the MRI. I had to ask the doctor twice to confirm that that was indeed my brother’s MRI on the wall.
David had a large glioblastoma multiforme in his brainstem. What he was describing as fainting when laughing out loud was pressure being put on the brainstem with Valsalva and shutting down brainstem function. Unfortunately, my prognosis was correct. He had a terrible brain tumor and only a few months to live.
After a biopsy, he received the best treatment at the time for that disease, which was radiation coupled with cisplatin. Futility was obtained quickly and by early June it was clear that he was beyond hope of a cure. He and his wife had their fourth child during this treatment regimen, and he had well over ten thousand people praying for him all over the world through his church’s network, and yet his health continued to decline. My wife and I were scheduled to graduate in July from our residency in Corpus Christi, and after the ceremony, we drove like the wind to San Antonio. David had been on hospice for a few weeks and was near death, slipping in and out of consciousness as we sped there.
When I arrived around 6 pm I saw David in his hospital bed, essentially in a coma, but he lightly squeezed my hand and seemed to mouth what he often called me, O’Kenny.
Sitting around David was his wife, my two sisters, my younger brother, my mother, and myself. We were a mix of somber and comforted, telling stories and occasionally laughing. As it approached midnight with my brother’s death rattle rhythmically sounding, we started recounting the stories of our time in Alaska. We started to tell the story about shouting “Hey Bear!” and laughed about the turtle that was David. We all laughed—the long and hard laugh of a family in pain together.
After a bit, just after midnight, we stopped laughing and settled into quiet. Total quiet, as we all noticed together that David had died.
There is much that is unknowable about the final stages of death. Many hold that hearing is one of the last senses to go, as some who have been in comas and recovered relay things heard while comatose. I believe David’s hearing was intact in those final moments. I believe he laughed, which pushed that pressure on his brainstem over the edge, and surrounded by love and family, my brother died laughing.
How do you want to die?
Do you want to die remembering wonderful moments? You won’t unless you make those memories and eschew working all the time. Do you want to die surrounded by love? Then live loving. If you want to die rich and unmourned, that too is in your grasp.
I want to die laughing.

Prisca Mbonu, Class of 2026
I learned so much that semester. I learned about the different ways a person can fall in and out of love, how to measure specific...
Read More
Prisca Mbonu, Class of 2026
I learned so much that semester. I learned about the different ways a person can fall in and out of love, how to measure specific heat capacity of a metal in Chemistry lab, the perfect step-by-step method to parallel park for my driving test, what medical specialty I would likely end up in after the grueling pre-med years and…about depression.
During that semester, I would become intimately familiar with the illness known as depression.
An illness that I had been largely unaware of throughout my life. An illness that I had brushed aside by the sheer will of what I often call “African stoicism,” a tough outer shell, impermeable to hardships and unperturbed by the twists and turns of life.
Depression? Who is that?
That semester. The lack of appetite. The loss of interest in life. The avoidance of friends and classmates. The skipped classes and missed meals. The unexplained sadness, unprovoked irritability, and unstoppable tears.
All signs pointing towards depression. All signs we could not see. All signs we would not see.
That is, until they became signs that refused to be ignored.
After endless probing and pleading, you finally confide in me. You tell me that you need help. That you have been struggling for a while. That you are sad all the time. That you don’t see the point of living anymore.
The last part breaks me.
You tell me.…you think you might be depressed.
It turns out that while I have had no experience with mental illness, you’ve had far too many. Enough that simply uttering the word “depression” elicits a visceral reaction.
You have experienced the shame and isolation associated with seeking mental health care. You have seen family members live silently with mental illness, afraid of whispered rumors and the inevitable judgement of others.
Unlike you, I did not grow up hearing words like depression, anxiety, and bipolar disorder. I am ashamed to say that I knew nothing about your illness at the time.
But I am determined to get you through this “hurdle.”
Straight A’s. Type A. A perfectionist. High achiever. This is simply another question to answer. A difficult but requisite college course to travail.
I do my research.
Exercise. We walk and walk. We talk and talk. Until our legs hurt and heels blister. Until we have exhausted both our words and our selves.
Diet. No more skipped meals. We are first in line at the cafeteria. A healthy breakfast to start the day. Lots of fruits and vegetables. Don’t forget to stay hydrated, always.
Music. We explore the rich music of my culture. I teach you the lyrics and dance moves. You marvel at the vibrancy and uniqueness of Afrobeats. I marvel at the fact that the music I took for granted could be so deeply appreciated by another.
K-dramas. We watch all the good shows, all the bad shows, and of course, everything in between.
School. We study together at our highly coveted spot in the library. You help me with art projects. I help you with Calculus I.
Everyday we live in this bubble of our own design.
Has the ever-looming cloud of sadness passed? Are you smiling more these days?
Or am I imagining the slight curve of your lips? Do I hallucinate the faint gleam in your hazel eyes?
I must have. Because you aren’t better. Distracted? Maybe. Not better.
We have been pretending that nothing is wrong. But ignoring an illness does not make it go away.
I am crippled by the fear that I can’t help you. That I am not enough. This thought terrifies me.
You are my roommate. Brought together by luck of a random draw and yet, you have become so much more. You are my friend.
I have learned to always push through obstacles, fearless and determined. But this isn’t just an obstacle. Your depression isn’t just a problem to be solved. A thing to bulldoze through with my endless optimism and stoicism. One more adversity to face boldly with my shield of resilience.
I bring up the next logical option. It’s time to seek help from a professional. Therapy, maybe?
You resist the idea. I knew you would.
But I persist. And reluctantly, you agree.
We walk and walk. But this time, we are not simply taking endless loops around a geese-invaded lake. This time, we walk with a purpose. This time, we walk to get you the help you need.
We walk, but don’t talk. Instead, we allow our minds to wander in an odd yet peaceful silence. And then I wait.
Your first counseling session is hard. But week after week, without fail, we continue to go. We continue to walk. I continue to wait. Now we have a new routine.
This time, you truly seem better. I am numb with relief.
Because in those months, I couldn’t tell you how scared I was. Afraid that our efforts would be inadequate. Afraid that you could sense my ignorance about your illness.
Thank you for letting me in. Thank you for getting out of bed at my insistence. Thank you for trying.
And thank you for allowing me to care for you.

Kavneet Kaur, Class of 2023
Character Description Kavneet: A naïve 3rd year medical student working a shift in a rural Emergency Department at the time of yet another COVID surge....
Read More
Kavneet Kaur, Class of 2023
Character Description
Kavneet: A naïve 3rd year medical student working a shift in a rural Emergency Department at the time of yet another COVID surge. Must work shifts for 28 out of 31 days this month. Tired, but ready to work and take on a challenge. Always hopes for the best and tries the see the good in a bad situation.
Scene: It is month 8 of 10 of my Emergency Medicine rotation and delta variant reared its ugly head.
====================================================================
[Cruising down the highway at the crack of dawn with the window rolled down, I let the cool, crisp air wake me up. The radio is screaming on repeat: “The death toll from COVID-19 is increasing day by day… Delta variant seems to have world leaders worried of yet another spike in cases”. As I pull into the parking lot, two deer cross in front of me near the entrance of the hospital. You don’t get that in the city.]
Hour 0
KAVNEET: “How is this shit still going on?” I grumble to myself as I walk over to greet my attending in the breakroom. I notice the tracker board with the list of current patients… just when I thought I was going to have a ‘Q word’ day.
“Q word” means “quiet”, but you don’t dare say that word in the ED unless you want all your staff cursing you out an hour later while being knee deep in patients that decided to take a trip to your emergency resort.
I overhear the overnight attending pass off a patient to my attending physician, who in disbelief remarked “This was the same patient I had on shift two days ago.” The patient is COVID positive and is currently waiting to be transferred to another facility for more intensive care, but no hospital nearby is accepting patients.
They have now been in isolation for more than 72 hours. Imagine a 6-foot by 6-foot room with white walls and no windows. No human contact outside of nurses coming in to give you meds or adjusting ventilator settings. Sedated. Looking more machine than human. Listening to the music of the vital monitor beeping similarly to a ticking clock, amid chaos happening in the room to the left and to the right of you. Lifeless.
It is quite literally the closest thing to solitary confinement without being imprisoned.
My trance breaks as we rush through the remainder of the patient list. I notice there are others waiting more than 40 hours needing to be admitted to the second floor for inpatient care.
Here’s the thing that the public tends to forget- there are still a portion admitted patients in need of critical care, who do not have COVID. This could be your grandfather having his first heart attack, your significant other that just got into a car crash or is having a miscarriage, or your child that is about to slip into a diabetic coma.
And the fact of the matter is that there may not be a place to put them or stabilize them. Even if we can, they are still left waiting for another hospital to “accept” them to get the care that they need.
Why does someone need to be interviewed to see if they are sick enough to be treated? How does that make sense?
Hour 2
KAVNEET: More patients are checking in. COVID patients get priority, especially if they have a below desired oxygen level. In other words, “priority” means you can be put in a room with an actual door that closes. What do we do when those rooms run out you ask? I pray to God. You pray to whatever Higher Power you believe in or just hope for some good vibes. “We have NO rooms open for COVID patients!” I hear the charge nurse scream as if it was not obvious. Though by the look in her eyes, more a scream of frustration than one to state facts. Let those prayers begin. We now have no option but to fill in these makeshift “rooms” with possible COVID patients. Picture a room divided into smaller sections by a shower curtain instead of an actual door. I try to justify it to myself as, “well, it’s not like there is any other place we can put them, and we can’t just stop seeing patients.”
Hour 3
KAVNEET: I do the best I can to help my attending and the staff see patients. At one point, I go to the front to help triage patients, some of whom had now been waiting for at least an hour. Our triage room is quite literally the size of a closet, so you can imagine how this was about to go.
With my head held high, a N95, surgical mask, and face shield, I march into the lobby and scream the first patient’s name to bring them into our broom closet. Yes, scream…it is that chaotic. I ask what brought them to our ED today. Cough, fever, shortness of breath? What a shocker.
“Have you been vaccinated?” I question with skepticism. No? Surprise, surprise. I proceed to get the vitals. Blood pressure 142/94… eh, won’t kill you, temperature 99.8… low-grade fever, heart rate 104… tachycardic, oxygen saturation 92… mildly hypoxic. Yep, this is to be expected. Ok now to swab for COVID.
Like clockwork, now onto the next one.
Hour 3.5
KAVNEET: We officially maxed out on the makeshift rooms, but we still have a lobby full of unseen patients. “What can we do? I understand we don’t have any space to put them, but we can’t turn them away,” my attending physician shouts through his N95 to the charge nurse as he rushes to check on a critical patient that just came in with low oxygen saturation. “PAGE RRT STAT”.
34-year-old female, with oxygen saturation in the 50s.
As my attending and others work to assess the gravity of the situation, the rest of us manage to add two gurneys and a chair… three extra spaces in the hallway of our small boondocks ED. If a code blue walks in through the door right now, we would literally be doing it in the ambulance bay outside of the hospital. Totally code compliant.
I rush back to the critical patient that was brought in. Everything and everyone moved like an assembly line. Prepare the meds, sedate, paralyze, intubate, get out. I open her chart and glance through it. She is a healthy young woman without any health conditions. She has had COVID-like symptoms for 2 days and began to develop shortness of breath overnight. So why is she this bad? Something is not adding up…Vaccination status? Unvaccinated.
As we exit the room, the front door almost knocks me down as the medical director of the Emergency Department darts in through the door. Before I can process, monitors start going off. BEEP BEEP BEEP! The patient that we just intubated… a bunch of staff rush in and one of the nurses’ pages RRT again. Oxygen saturation is 70. I stand outside the room as I see the panic in everyone’s eyes. There’s simply no time for this right now.
My attention diverts behind me as I overhear the charge nurse and medical director calling hospitals from DFW to College Station to find beds so they can move our current patients out to add new ones to the trenches. The medical director even made a personal call to the CMO of the hospital system. Little did I know that in the last several hours, we were still getting calls from the transfer center to accept patients from Kansas.
Hello? What happened to the entire state of Oklahoma?
Hours 4.5 to 9
KAVNEET: We come up with a plan to open a currently unused space on the second floor to put some non-COVID, lower acuity patients. One of the nurses told me this is the first time since the pandemic began 1.5 years ago this was being done. And for the first time since beginning my shift, I force myself to find a moment to stop and take in what is going on around me.
Do you think if an unvaccinated person saw face to face what it looks like to have more than a “COVID cold”, they would change their mind about getting vaccinated?
I often think about that young lady on the vent. If she made it off, her life will never be the same.
On a systemic note, I’m still trying to grasp how we got here? I see nurses, techs, RTs, pharmacists, radiology techs, and physicians running around the hospital trying to do the best they can, trying to solve problems that were created by this system, trying to juggle tasks out of the scope of their practice on top of their normal duties because there is no one else there to do it. I am appreciative of how hard each team member worked in our small ED that day. They are the true embodiment of perseverance and fight.
On top of dealing with a public health crisis, the unfortunate reality of working in a small ED such as this one is that patients are at risk of dying, simply because they cannot get to another facility for more intensive care. Bigger city hospitals will not accept more patients because they are also being bombarded with COVID, and statistics show that most of these patients are also unvaccinated. Even then, at least the bigger hospitals are equipped with resources and specialists to handle the surplus. To put it into perspective how smaller, boondocks EDs are affected, if you are unfortunate enough to come on the wrong day, your options are to talk to someone through an iPad or get transferred to another facility that has someone physically there to take over your care. Often, it’s the latter and we are 40 minutes from the nearest big city hospital.
If being vaccinated means less stories like what you just heard, less burnout for the people who are tirelessly and endlessly taking care of you and your loved ones, less loss of the ones you hold close to you and heck, maybe even you yourself. The question I then pose to you is: If you do not have a legitimate medical reason to not get vaccinated, what is the hesitation to get the vaccine? Whether you are pro-vax or vaccine hesitant, we can all agree that we are mentally and physically tired of this and want life to go back to “what it used to be”.
====================================================================
**This piece was a finalist for the inaugural production of Stethoscope Stage

Sarah Cheema, Class of 2023
Sometimes I don’t know if I can handle another one. Another uncomfortable pause, another sudden shift in body language, another dance of “did you get...
Read More
Sarah Cheema, Class of 2023
Sometimes I don’t know if I can handle another one. Another uncomfortable pause, another sudden shift in body language, another dance of “did you get the vaccine” and “no, it was too quick,” “no, I don’t know what’s in it,” “no, and I will not.”
I wish it were just a simple question and an answer – like all the other checklists in my patient visits. I can ask a patient about their home life, diet, drug use, and sex life and get an answer so nonchalant I have to double-check that they’re listening. But, the same person might nearly freeze when I ask about the vaccine. It’s almost as if I can see their spine straighten and their muscles tense, prepared for Battle with the Know-It-All Doctors (and their Students). Their walls come up and suddenly we are miles apart. That’s what I hate the most. Not even the uncomfortable conversations, but the sudden distance, the instant formality as if it is no longer two people speaking in a tiny room but instead, a hot-seat interview on a news channel.
This is not to say they are all the same, they are definitely not. There are those genuinely seeking information, truly torn between a desire for safety and a fear of complications unknown. There are those paralyzed not by their own fear, but their daughter or sister’s fears. There are those with bookmarked Facebook posts, ready to brandish a vaccine horror story like a knife. There are those who I wonder about the most. Those who strongly and firmly state “no” and offer no further engagement. Then, there are those who I feel like begging. The 34-year-old pregnant woman, the diabetic 65-year-old headed for dialysis, the elderly 83-year-old in the emergency department. With them, I walk the thin line between persuasion and disillusionment, hoping I don’t trigger the dreaded blank stare. I think of my unfortunate patients. The 31-year-old guy who was finally cleared to go home after a 60+ day hospital stay, only to suddenly pass away from hospital-acquired COVID 1 day before discharge. Sometimes, I refuse to walk the line at all and I simply move on.
Honestly, it all depends on the day. On good days I feel kind and patient, mindful that we all crave the same health and freedom. Other days, I am tired and frustrated. Tired of all the cracks in the system, like the fact that students aren’t supposed to see COVID positive patients yet I spent countless days in the ER listening to the lungs of patients incidentally found COVID positive 15 minutes later. Tired of spending my days as a medical student next to a doctor on a laptop telehealth visit instead of floating between exam rooms as my predecessors did. Tired of the relentless acne from wearing a mask for 8-12 hours daily. On these days, my brain reverts to its primitive schema mode and determines the status of each person: either With Us or Against Us. I know, I know that this is not the reality. I know that everyone supports healthcare workers and vaccine hesitancy is remarkably multifactorial. Still, compassion fatigue is real and it permeates hospital halls like its own disease.
I try to imagine what the vaccine is to them. Often, it seems impossible we are talking about the same thing. What is to them a dreaded and dangerous trap is to me a golden ticket, a precious shield in a chaotic war zone. It absorbed some of the helplessness that we were drowning in. It gave me a guiding light, a dream of an education unmarred by a new virus. The “truth” outside the politics, fear, and hopeful dreaming, probably lies somewhere in the middle. The vaccine is neither a magical cure-all nor a manufactured lie. It is just a little piece of nucleic acid that travels into cells to become a protein that WE HOPE MAKES A DIFFERENCE.
====================================================================
**This piece was selected and performed at the inaugural Stethoscope Stage production in 2022**

Shanice Cox
Written & Performed by Shanice Cox [audio m4a="https://mdschool.tcu.edu/wp-content/uploads/2022/05/Take-a-moment….m4a"][/audio] Take a Moment Chapter I: Obstetrics and Gynecology Take a moment... to breathe Take a moment...to...
Read More
Shanice Cox
Written & Performed by Shanice Cox
Take a Moment
Chapter I: Obstetrics and Gynecology
Take a moment… to breathe
Take a moment…to seize…this moment that sits before you
Take a moment… to see,
beyond the gown, the drape, or the anatomy
Take a moment… to listen to the history,
To the crackles in her speech, to her hesitation,
To the hum in her pause, to her tone’s vibration,
Take a moment… to view
What it is that lies in front of you
As her hand is carefully positioned behind her head,
And the gown is respectfully placed,
while ribbons gently touch the side of the bed,
and the slight embarrassed flush of her face
Take a moment…to view
the contour of her breast
Clockwise and counter
view symmetry, asymmetry,
are you still there?
Or has she become a mindless exercise of your checklist,
color, texture,
Are the nipples inverted,
Is discharge produced,
are nodules immobile,
is her quality of life reduced?
Take a moment… to be silent
With differentials and questions and familial history pooling in the mind,
For you must make space in this stillness of time,
To deliver a news that may shift the course of this rhyme
Take a moment…to reimagine,
That this couldn’t be you,
That you couldn’t be the one
To look in her eyes and deliver the troubling news,
It was the life you wanted,
The only specialty you knew,
But over the course of your training,
The weight of this burden grew,
Take a moment…to revisit
Those feelings that once were,
Filled with such promise,
That now feel so obscure,
Take a moment…to gather
Your thoughts,
your desires to serve in this space,
To counsel, to teach, to empower, and to share a thoughtful embrace,
To right the wrongs of centuries-old medical practice
With dignity, humility, and grace
You approached the field,
With only the thoughts of positive outcomes,
But failed to consider…when there wasn’t one,
Your story did not capture the woman who fell ill,
Or when the fetus had been delivered,
Cold, pulseless, and still
Take a moment…to process
How you revered in maintaining the health of the womb,
But after seven days on the service,
This vessel of life,
Evolves into a hollow, pear-shaped tomb,
Take a moment….to reconsider,
What life would be if you made more room,
To till the soil of your garden,
And allow for the seeds of destiny to bloom,
Take a moment…to look
Into the mirror and see what you’ve become,
Because there in that reflection,
There is a slight resemblance of someone,
Fragments of the old, but glimpses of the new,
Moments that reflect past passions,
but notes of what they had morphed into,
This desire to serve extended farther than that of the woman’s womb,
And in this infinite Eden of possibility,
My brainchild found room
Chapter II: Urology
Take a moment…to reset
To look at this rotation anew,
Because what you had been searching for,
had somehow found you,
It began with a knock on the door,
And a sheepish reply “You may enter”
Unconsciously I shift my attention to the woman,
But she is not who sits at the center
Take a moment…to view,
The air of defeat in the slouch of his posture,
Take a moment ….to recognize his courage to seek a doctor,
He peers up at you,
An emptiness in his gaze,
His wife quickly rushes over to hold his hand,
To somewhat mask the depth of his dismay
He tells me of their journey,
And how they’ve tried for years and years,
Until they sought the help of medical professionals,
Who would somehow ease their burgeoning fears,
He spoke of her strength,
Navigating conversations about her ability to conceive,
He spoke of her courage,
To defend and protect her family without reprieve,
Take a moment…to notice
The pain that continues to resurface,
And all that they had been through,
The waning support of their loved ones,
The constant judgement and ridicule,
Yet she sought answers,
she completed all the tests,
But when they all came back normal,
She entrusted him to do the rest,
Take a moment… to breathe
Take a moment…to seize…this moment that is before you
Take a moment… to see,
beyond the gown, the drape, or the anatomy
Take a moment… to listen to the history,
To the crackles in his speech, to his hesitation,
To the hum in his pause, to his tone’s vibration,
Take a moment… to view
What it is that stands in front of you
As his hand is carefully positioned atop his head,
And the gown is respectfully placed,
while ribbons gently touch the side of the bed,
and the slight embarrassed flush of his face
Take a moment…to inspect
the meatus and penile shaft,
Testicle, epididymis, spermatic cord,
Give yourself this moment to perfect your craft,
Are the testes symmetric,
Is discharge produced,
Are prostate nodules immobile,
Is his quality of life reduced?
Take a moment…to reimagine,
That this could be you,
That you would someday be the one
To look into his eyes and deliver the hopeful news,
It was the life you wanted,
Combining the admiration of a specialty you once knew,
Yet a new seed was planted,
With a flourishing destiny coming true.
====================================================================
Artist Statement:
This piece is dedicated to my grandmother, Claudette Cox-Brown, who exposed me to the intricacies and
delicacy of reproductive health. She served as a nurse midwife in Jamaica, England, and New York and shared with me so many
precious narratives of femininity, obstetric care, and the hardships of navigating pregnancy whether wanted or unwanted in
years past. Over time, the initial intrigue of her stories sparked an interest to pursue a similar path, and it followed me for a large
portion of my life. It paved the way for research opportunities in college focused on breast cancer, a medical mission’s trip to
Durban, South Africa focusing on the obstetric care of mothers and babies affected by HIV, my first career as a medical assistant
at an OB/Gyn office in Washington DC, and even the acceptance of a medical fellowship whilst in medical school, and for that I
am truly grateful.
However, this dream of mine to be an OB/Gyn never included the emergencies that happen in the delivery room. And
when things go awry, it happens fast. In my many experiences, I had always seen the outcome of healthy mother and healthy
baby, but never considered the possibility of losing either. My time in the longitudinal clerkship exposed areas of my journey that
I seemingly avoided, or hadn’t been privy to, and placed me in an emotional headspace I couldn’t escape. The beloved field that
had my heart for so long, had cemented wounds that had me question what the next step would be. In this poem, I address
some of those hardships, but also this love that I have for reproductive medicine transforming into something more, something
that created a space for old passions, but hopeful futures.
Urology has been that great awakening for me, not that I had slept through the life of undergraduate medical
education, but just an opportunity to see things both old and new with renewed purpose. Traits and behaviors that I had
perfected in my pursuit of being an obstetrician, have crafted my mindset about practicing urogynecology. I feel hopeful that my
interests in gynecologic procedures that focus on health after childbirth such as pelvic floor instability and urinary incontinence,
along with surgeries with the intent to tackle conversations that have are attached to social stigma such as female genital
mutilation and transgender medicine, can be cultivated in this field.
This poem takes you on that journey with me, the journey of facing those emotional hardships with the patient, and
within myself. Take a moment was written as my reminder to find some time, even just for a brief moment to be in that moment.
It is a mantra I use to escape my racing thoughts, to reconnect with patients, to observe, to reflect, and be mindful of the here
and now and sacredness of the space that my medical journey has afforded me. Take a moment though dedicated to my
grandma is a thank you to each obstetrician/gynecologist, midwife, nurse, charge staff, medical assistant, phlebotomist, practice
manager, and sanitation engineer that inspired and prepared me to seek and gain knowledge about every aspect of feminine
health. It is also a commitment to each urologist/urogynecologist, resident, and therapist who have accepted, mentored, and
exhibited patience and support as I worked to figure out the journey that lies ahead.

Shelby Wildish, Class of 2023
Character Description: Medical Student. Female. Late 20s. Eager to learn medicine, self-critical about self-expectations, general baseline tiredness. Wearing hospital issued scrubs, white coat, old worn-out sneakers....
Read More
Shelby Wildish, Class of 2023
Character Description: Medical Student. Female. Late 20s. Eager to learn medicine, self-critical about self-expectations, general baseline tiredness. Wearing hospital issued scrubs, white coat, old worn-out sneakers.
Scene: In Medical Student’s apartment living room. There is a big, colorful, soft chair with armrests in the middle of the room. Beside chair there is a standing full-length mirror. In walking distance from chair is a table, with a lamp, a cell phone, and a laptop computer. There is a rug on the floor and a small footrest.
====================================================================
[Enter Medical Student – she walks towards a chair, stops, turns to face mirror. She looks exhausted.]
MEDICAL STUDENT: You did it. You’ve made it to the end of another busy day. (Moves to sit down in chair, pauses to look down at feet) Damn, my feet hurt. I don’t know how Dr. Barterman does this all day. Walking up and down those long emergency room hallways, never getting a chance to sit down. It’s her shoes, has to be. She has some of those fancy clogs I’ve seen other docs wearing. I need to get a pair. Well, one day…(looks at old sneakers, then up at audience, shrugs)…when I can afford it.
Time to reply to the messages that came while on shift. I bet it’s the college roommate group chat blowing up about the recent girl’s Facetime chat. Another hangout without me; more group memories made without me. I find it interesting how quickly during quarantine it became the “norm” for social interactions to be almost entirely through computer or phone screens. Just shows human adaptability I guess… (Sits quietly, scrolling on phone, to self) I don’t even know what the update is about Amanda’s baby or Susan’s postponed wedding plans. I really need to call them – add that to the long To Do list.
(Looking at phone, slowly smiling then laughing aloud) I can’t believe they remembered that story! That was so long ago.
(Directed to audience) So, once I was dared to jump in frog fountain and then slipped while on the wall and fell face first into the water. (laugh, looking back to phone, nostalgic) we were all such idiots in undergrad. Such fun, but such idiots. I wonder what brought that up in the chat? (directed to audience) It feels good not to be forgotten. I remember this one time that Amanda, Susan, and I snuck into my brother’s house and stole his car during a snowstorm. Us three freshman girls, just trying to do some car drifting in the supermarket parking lot. I definitely need to remind them about it. (start typing on phone, to self) Too funny. (phone dings with notifications, medical student sits quietly, smiling and typing replies to the group chat.)
(Smiling, student puts phone down, looks off into the distance, demeanor changes to one of concern. Look around room, pick up phone and begin typing)
Guys, did you hear about those mass graves for unclaimed patients on an island near New York City?
(sits quietly)
(Irritated, speaking to audience) How can I be laughing when such things are going on in the world? I should be reminding my friends about the situation at hand. Bringing the conversation back to the patients, back to the families, back to the healthcare workers and back to COVID-19. (stand up, pacing and talking to self) Remember your reality. Remember the world’s reality. You wake up each day, and are reminded through new articles, research journals, social media posts, videos, and patient stories of the one sole focus – COVID. Don’t forget it has caused schools to close, businesses to shut down, economies to crash and nations to close their borders. It has caused millions to become unemployed, thousands to become overworked and all to become fearful. It has killed. It is killing. And it will continue to kill.
How dare you laugh? How dare you forget momentarily. (phone dings, student walks back over to the chair, glances at it, reads it, places it face down on armrest of chair, without replying.)
And you, you underestimated this virus’s capability, initially nonchalantly saying {in a mocking voice} “Oh, it’s just another influenza-like infection.” You felt a need to have a reassuring answer for concerned family members. When really, what you should have just said: “what do I know, I’m not even finished my second year of medical school.”
You incorrectly, and almost arrogantly, claiming it only affects the elderly and immunocompromised. Have you temporarily forgotten that you have three grandparents? Think of Nana, of Papa, of Grandma. This virus could take them from you. You are guilty of blissful ignorance. How lucky are you to be so far disconnected from any serious, immediate personal consequences that you have the luxury of having moments where you forget about everything, all things COVID-related. You’re lucky. Your family has been safe. Many families can not say that.
(walk slowly back to the chair, sit-down, pick-up phone and begins speaking while typing) The first patient this morning was a pleasant young guy, maybe 30. (To audience) Not that bad looking either. (back to phone) When we saw him, he was making jokes, laughing, even flirting with nurse Kelly… But you could tell he was having a really hard breathing. (To audience) His face was so pale. (back to phone) We got his oxygen levels. It was 86%. Dr. Barterman thought it was COVID and admitted him to hospital. That’s bad news.
(put phone down, stand up, start walking over to the table, stop, to audience.) At the end of the shift, we heard he wasn’t doing well. They found pneumonia in both lungs. He would probably need to be put on the ventilator. And the crazy thing, he doesn’t have any chronic medical problems. He runs marathons. He doesn’t do drugs, doesn’t smoke. He hangs out with his friends, has a dog. And before the quarantine, loved exploring the city. He is a healthy guy. Well, was a healthy guy.
Was a healthy guy.
(continue walking to table, pick up computer. Walk back to chair, sit down with closed laptop on lap.)
I can picture him, before all this COVID stuff, with a group of friends at a brewery. Joking around, laughing. Maybe even having one of those moments when you laugh so hard that you almost fall off your chair in joyful pain. I bet he is the type of guy that looks for the good in the moment. I bet he would tell you not to beat yourself up about reminiscing, almost as if encouraging you the laugh. You feel the sad, the guilt, the hard times, he would want you to feel the good too.
Isn’t that human nature? To feel. Emotions protect against apathetic eyes. Apathy has no past to base experience on. From feeling nothing for nothing, is no life at all.
(pause, look off in the distance for a while. Then re-center, and open laptop, click on a few buttons, slowly read out loud as if reading from phone) The FDA has approved the COVID-19 Pfizer vaccination.
Could this be it? A light at the end of the tunnel. A chance to get some element of normalcy back in life.
(stand up, beginning dialing on the phone, lift phone to ear, pace around) I have to get it. I need to get it for my family, for my patients. I need to get it so I always remember. Remember what COVID has done… what COVID is doing.
Hello, Dr. Barterman. Hi. It’s me, Savannah… Yes, I just saw the news article… I know! … Yes, it’s all so exciting! … It’s what we were hoping for… I can’t wait for when I can get it. Can you help me register? … Great, thanks … Of course I remember him… he what? … when? … Thank you for telling me.
He was healthy… was.
====================================================================
**This piece was a finalist for the inaugural Stethoscope Stage production

Patrick Powers, Class of 2024
Sometimes, it is nice just to sit and listen to the wind rustle the leaves. The cooling temperatures linger in the air like a prelude...
Read More
Patrick Powers, Class of 2024
Sometimes, it is nice just to sit and listen to the wind rustle the leaves. The cooling temperatures linger in the air like a prelude to the winter ahead. I never thought I would find myself here, and I cannot help but smile through tired eyes. How many times have I missed the movement of life around me because of the movement around me? The enigmatic distractions surround us, poisoning the purity of the simple beauties of life. I admire the leaves in the fall. Of course, their color change inherently captures my attention as a reminder to stop and ‘smell the flowers,’ in a similar way a set of olive-green eyes might remind me to sleep, remind me that I have to eat three times a day, to try not to clench my teeth, and that, really, it will all be ok. In the end, there is an undeniable elegance to the falling of the leaves; a gentle but self-assured poise to each and every leaf that, when the time is right, plucks itself from its roots, and bravely sets sail on its solitary, yet sui generis voyage. The time must come for all leaves to embark on their journey, and though the trek may route through a previously undiscovered, and albeit, arduous, path, just as one cannot stop the leaves from changing colors, this too, embraces its own inevitability. How valiant, to stare down the fear of falling, to trust the make of their ship, to sail alone. Their destination is clear, their conviction clearer. The winds may blow, swaying their ship, aggressively rocking the foundation in an unrelenting manner. But, clever as the leaves are, flow with each windy blow, like water around a stone, never deterred from their ultimate goal, but ebbing gently with each test from the wind. No matter how hard the winds may blow, how laborious each challenge may appear, or how many bruises each leaf must endure, just as one cannot stop the leaves from changing colors, this too, embraces its own inevitability. As the leaves quietly, yet confidently, make their way to the ground, leaving behind the branch which had been their home for so long, so too must we all embark on our own journey. Which then begs the question, what is the ground? What is the ultimate destination? Worry not, the end is neigh. Rather, memento mori, only in as far as it gives purpose to life. For what is light without darkness, peace without war, and love without hate.
Perhaps I, too, can learn to be more like the leaves. The fears seem insurmountable, of being left behind on the tree, of falling, of never having the grit to jump when my time comes, of oblivion, cascaded by volume of inexplicable worries that flood every available space in my mind. I am sure the leaves feel similar. How beautiful that expedition must be, though, I think to myself; to experience those tests of life. The wind, with its capricious and fickle self, brings the blowing challenges that provoke us to breathe deeply and suck the marrow of life with each deliberate adventure. We are all meant to thrive so Spartan-like yet gentle, as the leaves do, staring deep into the eyes of falling, knowing we were made to live the life set forth in the path that is unraveling itself before our very eyes, that the make of our ships can and will endure the journey, and to jump, bravely and boldly, heart racing, with a smirk. Perhaps that smirk is to spite the inhibitions, perhaps it is because of the joy of finally jumping from our branch, or perhaps both. Sometimes, it is nice just to sit and listen to the wind rustle the leaves. I cannot stop the leaves from changing colors, and I cannot stop the fear that lingers in my mind. When I think about it, none of that even matters. My heart could flutter, butterflies flapping in my stomach, as I wipe the sweat from my brow. What matters is that we jumped anyway. We jumped off our branch, flying into our odyssey, highs, lows, and in-betweens, tears, laughs, and far too many unforgettable memories to recount, living the life we were meant to live, so that when it comes time to meet the ground, we will not discover that we have not lived. So here we go, with ill-fitted blue scrubs, a set of scuffed-up clogs, and a little too much caffeine, I catch a glimpse of myself in the sliding front doors of the hospital; tired-eyed smile as I sneak back into the resident’s lounge, just a leaf, riding the wind.

Peter Park, Class of 2025
When I was little, I spent my pre-teen summers with my grandfather in Korea. He was a retired salesman who spent his time coaching the...
Read More
Peter Park, Class of 2025
When I was little, I spent my pre-teen summers with my grandfather in Korea. He was a retired salesman who spent his time coaching the local high school soccer team. In the hot, humid summers, he would coach me in an equally intensive sport: gardening. His backyard spanned half an acre of trees, ferns, and cabbage. But his most labored love was his grapevine. Together, we built fences eight feet tall, allowing for her to expand her leaves reaching for the sun. She protected me from the heat like green clouds in the sky, dropping sugary fruit from the heavens.
One day, my grandfather handed me garden sheers with large rusty blades. He said we would prune vines that day. Unsure of what pruning was, I followed his direction: cut each branch he pointed at. My sheers would slice the darkened bark and reveal a white-greenish core, where glistening sap dripped at the center. The grapevine’s branches would fall to the floor with a thud and all the grapes would scatter like marbles.
My grandfather pointed to various branches of the vine, “This one is infected. This one has been eaten by insects. This one is too small.” I nodded with each response but could not understand the differences between the branches we cut and the ones we spared.
We came onto a large branch that was sturdy and strong. Its bark was like the thickness of a tree and would not break under my grandfather’s bare hands. I prepared to move on to the next branch until my grandfather placed his hand on my chest. He pulled me to the branch and said
“Look, it’s dying.”
I was confused. “How? It’s so big. It must be alive.”
He considered, “You’re right. It is alive and growing well. But, if we allow this one to grow, it will steal the energy from the main branch, and go in a different direction. That’s not where we want to take it.”
For the first time, I saw the grapevine as one connected system, and I understood. This sturdy branch deviated almost exactly at a 90° angle. Like a rebellious teenager, she wanted nothing to do with her parent. Allowing this one branch to grow meant the entire grapevine would die. Her growth would be her downfall.
My grandfather noticed my childish stubbornness and assured me that this was for the whole grapevine. It’s better this way. Not wanting to cause trouble, I moved on and began to squeeze with all my might to cut this rebellious branch.
Snap!
Fluid began to pulse out of the old artery with an almost desperate will. I put away my scalpel and began to sheer away more of the fat deposits surrounding the heart. Years later, in the cold air of a cadaver lab, the grapevine had taken shape, manifesting itself into an aorta branching into its capillary beds. I dug a blunt tool underneath an artery, pulled it towards the surface, and deciphered its Latin name: External Carotid; Subclavian Artery. As I followed the arterial branches, I snapped the artery in two, suspended in air with no grapes to fall.
Once again, I viewed all the blood vessels as one connected system, and I understood. My cadaver died from a stroke, specifically from cancer that had both blocked the brain’s artery and redirected new arteries for itself. This was the sturdy branch who became greedy, stealing the energy from the main branch. Her growth became her downfall.
That night, I got a call from my family stating that my grandfather had passed. He had died in his sleep. We learned that “dying in your sleep” is most often because of a dysfunction of the heart, that, for some reason, simply ceases to pump.
You would think that his body might have learned from his years of pruning. That he would know which branches were to be cut and which were to be spared. You would think that I would have remembered to return his calls.
I wondered who would care for the grapevine now. How she could grow without her pruner? Would she meet the same fate as my cadaver?
Many years ago, I asked my grandfather, “what will happen when the grapevine dies?” He turned to his vineyard and reached out, picking off one of the green grapes. He showed it to me, “Even if this grapevine falls, its sweet grapes scatter out leaving sweet memories with everyone who eats it.”
He tossed the grape in the air and I caught it in my mouth. The taste of sweet memories.

Henri Levy, Class of 2024
The man on the table was a stranger to me as many patients tend to be in healthcare. I had never heard his voice nor...
Read More
Henri Levy, Class of 2024
The man on the table was a stranger to me as many patients tend to be in healthcare. I had never heard his voice nor seen him awake. He was already prepped and draped in the typical sterile fashion ready for his liver transplant. Although I had never met him, I knew several scraps of information about this person. I knew that he had a MELD score of 39; without this new liver, he had over a 50% chance of mortality within the next 3 months. I knew that this operation had the potential to extend his life by many years, decades even. I knew his family was waiting to hear how the surgery went.
Approaching the table, I examined the yellow stomach sticking out from the blue tarp marked with a large, backwards L indicating where the incision would be made. Steel and electricity unceremoniously made short work of the previously untouched muscle, fat, and blood vessels. The surgeons peeled back layer after layer, made suture after suture to control the destruction they were causing to extract this rubbery, bumpy liver. This was not my first time spectating during a surgery–nor will it be my last–still, I could not help but wonder about the role of pain in medicine as I watched these well-choreographed events unfold. How could therapeutically hurting a patient play into the role of being a healer?
I think everyone who goes into medicine wants to help people who are suffering. The idea of being the source of that suffering seemingly goes against the vow of beneficence and non-maleficence providers take. In a much less theoretical sense, it makes me uncomfortable to hurt someone even with good intention and sound reasoning. Take, for instance, minimally invasive surgery. We are told that laparoscopic procedures are lighter on the body and yield quicker recovery times. I remember one patient describing feeling like he was just beat up by a bunch of baseball bats after his robotic gallbladder removal. Statements like that put larger, more aggressive procedures into perspective on how a patient feels afterwards. Imagine how someone must feel after an hours long open procedure — the kind with midline incisions that are the full length of the abdomen. This does not even include the anxiety someone might feel just having to go into the operating room for a surgery. Suffering is not limited to surgery either. Medicine is rife with discomfort and pain due to various procedures that range from benign to absolutely life changing. Range of motion tests cause patients with rotator cuff injuries and muscle sprains to wince. Medications we may prescribe can have severe side-effects. It is not uncommon to break life changing news to patients and families causing stress and psychological suffering well beyond just one individual. Inducing some level of discomfort for the patient is common as a physician. Yet all of these, and more, would be considered standard practice. It seems that many of our solutions require things to get “worse” before they get better.
Perhaps what makes this whole concept so strange to me is the idea that it will not be long before any one of us in my class will be expected to do these things. I find myself wondering who am I to inflict this pain on someone? I am just one human in a room, hoping to have letters behind his name someday, trying to practice medicine on another human in the room. In any other context these incisions, maneuvers, and causing general psychological stress could be deemed illegal or at the very least unethical. In a hospital they are expected. Patients trust doctors to do what is best – even if that treatment comes at significant personal cost. That burden becomes even heavier when realizing that there will be suffering no matter what happens. The question is just how much will occur. The 4-year medical school curriculum and 3-year minimum residency training are both testament to the fact that these practices and procedures are anything but random. The gold standards are tried and true in improving people’s lives. We will all be highly skilled after our training is complete – a knowledge built on an infinite series of trials and errors. Still, despite the current triumphs in medicine, outcomes are not always predictable despite a physician’s best efforts.
I saw firsthand how extreme this iatrogenic suffering can be. Unfortunately, this liver transplant case was one of the rare instances where the patient did not survive the procedure. He tragically expired on the operating table despite enduring more than five hours of surgery and multiple rounds or brutal CPR. He did not even get to use his new liver since blood flow was never established. Seeing that chaotic scene will stick with me forever. No errors were made. Everyone involved was highly skilled and competent doing the things they have done hundreds of times before with great success. Seeing everything unfold opened my eyes to just how little a non-medical person knows about the almost violent nature of medicine at times; ignorance is bliss. Liver transplants have a high success rate. 75% survive the first five years after their operation. This is a marked improvement from the mere months this man had without this donor organ. As with any procedure though there are implicit risks that need to be balanced with any potential gain. There were high stakes with the procedure. The decision to proceed was the correct one; to get this new liver was to live for many years to come. Yet had the family known he would not survive, or had they seen the extent of the damage inflicted on his body from advanced cardiac life support, perhaps they would have simply chosen to enjoy those last few months with him instead. Hindsight is always 20/20. It may have been his alcoholic cirrhosis that brought him to the table, but it is hard to shake the feeling that it was medicine that killed him.
Stitching up a recently deceased person is a strange sensation. Perhaps stranger though was the sense of closure it offered with the situation. Medicine is not perfect and our means to achieve our goals can be savage. Yet, we are doing our best with the odds ever stacked against us. We work hard to ensure that people suffer to the least extent possible. Situations may go from bad to worse, but the intention is there and the knowledge and skills backup every decision that is made. Yes, suffering is inevitable, but surely it can be minimized. Just like with this man before me, the sutures were a feeble, but well-meaning attempt to make things better. Ultimately, it makes me think about the role of striving to do better as a physician and a person. At the very least, he will be presentable for his family to see him one last time.

Matthew Pagano, Class of 2024
A mother and son duet. Mom draw her staff, Linea nigra noting her fertile tune Blue lines track his song, and purple hers. Yellow...
Read More
Matthew Pagano, Class of 2024
A mother and son duet.
Mom draw her staff, Linea nigra noting her fertile tune
Blue lines track his song, and purple hers.
Yellow contractions, thunderous cymbals
Time for the concerto to close, burgundy drapes to be drawn
and a new solo to begin.
Intermezzo
Blue absence
He won’t play, their performer is listless
a much crasser show must begin.
Hands clasped, like sterile prayers given
Mentally reciting verse from text, medical bibles.
Expectation of what is to come.
Human hope to be the unwritten exception, an unforeseen statistic.
Gospel gives way to staccato
cutting
ripping
tearing
and
Silence.
no cry, no croone.
Red, iron metal, bloody, crimson afterbirth
A former home, the drumming of maternal’s love
a welcomed cacophony
giving way to
Silence.
still.
discarded tissue.

Tom Deas, MD, Physician Development Coach
Resilience by Peggy Godfrey No promises the wind will make Unto the tender grasses Nor leave a trace or memory Nor count the time that...
Read More
Tom Deas, MD, Physician Development Coach
Resilience
by Peggy Godfrey
No promises the wind will make
Unto the tender grasses
Nor leave a trace or memory
Nor count the time that passes.
In gentle breeze or howling storm
Passion ebbs and flows
Resisting not, the grasses bend
Tremble, sing, and moan.
Without the wind the grasses
Never have a chance to know
Their grace or range of motion
Songs of joy or woe.
As though in battle with the wind
The lifeless creak and grown
Stiffly clattering in the breeze
To break beneath the storm.
But, oh, to watch the living
Bid welcome to the wind
Wind and grass so separate
In union once again.

Peggy Godfrey is my exceptionally talented sister, Colorado rancher, and respected cowboy poet who has published four collections of her authentic cowboy poetry and prose including Write ‘em Cowboy (1993), Write ‘em Roughshod (1994), Write Tough (1995), and Stretchmarks (2003). Resilience is one of my favorites. The visual and auditory imagery of the grass and the wind reveals Peggy’s keen observation of nature and awareness of her environment. More importantly, she reflects on her life experiences which have ebbed and flowed as the grass bending in the wind. Her lyric captures this certainty: without stress, we cannot develop our full potential of “grace or range.” The weak, rigid, and inflexible, unable to learn and adapt, will fail in the storm.
Resilience is the ability to endure, recover, and grow stronger in the presence of adversity. All worthy endeavors, especially medical school, residency, and the life-long role of physician require resilience. We confront adversity and endure; face failure and recover; accept the “no’s,” adapt, and become stronger. Brilliance and skill alone are insufficient to sustain us through training and medical practice. Like the grasses, we must “bend, tremble, sing, and moan” to find our “grace or range of motion” in our “times of joy or woe.” It is no coincidence that Coach Thu and I are paired in Team Resilire. My sister and I were truly blessed, as children and well into our adult lives, to learn to be resilient from a father who lived to 104 years.
Our father was the personification of “The Greatest Generation” and a gold standard role model for resilience. He was a small-town boy from Arcadia, LA, who in his teens endured The Great Depression of the ’30s. He attended Louisiana Tech at the age of 16, playing football and boxing. He subsequently attended medical school at LSU School of Medicine in New Orleans where he met “Scooper.” They married in 1941 – the same year he was called up to serve in the violent WWII battles in the Pacific. He served as a front-line physician in the Philippines Islands. Despite the grave adversities of war, he advanced to Regimental Surgeon and earned the Silver Star, Bronze Star, and Presidential Unit Citation for leadership and uncommon valor saving wounded soldiers under fire. Later in his life, he treasured the reunions with “my boys” the dozen or so remaining medics who were in his command during WWII.

After the war, he completed another two years of residency training before becoming a family physician in Homer, LA in 1947. (Tom, Jr arrived in 1948.) It was a difficult and demanding life of frequent house calls day & night, superimposed on long hard days in the office and hospital. In establishing his medical practice and as a community leader and moral voice, he faced adversities with wisdom and grace—enduring, recovering, and growing stronger.
As a child, I felt no calling to medicine – a difficult profession that demanded so much of my father. I recall thinking, “I never want to work that hard.” However, he thrived in the joy of his intense physician work-life. He was also a prolific writer, reflecting often in prose and poetry on life’s joys and sorrows. His reflections encompassed his World War II experience, my mother – “Scooper,” the love of his life, family, and his role as a small-town family physician, community leader, and man of faith. His passion for medicine, joy in his work, and his unconquerable resilience were ultimately the reasons I altered my choice of profession from research chemist to physician four years after college graduation.
Here is an excerpt from a letter I wrote him in 2014 when he was 98-years-young and I was just a kid of 66:
Dad, I cannot tell you how much it has meant to me to have you as a model of a caring physician devoted to your patients and profession. I share your enthusiasm for the diagnostic challenge. It has been such a satisfying career. I cannot imagine my life if I had not found my way to medicine. For that, I am most grateful to you and your great example. I treasure the notebook that you prepared in 1946 to start your practice which summarized the current therapies of the day. A chair from your office waiting room is in my home study to remind me of your successful medical career as a beloved family physician.
My Dad died in May 2020 at the age of 104, my father, my role model of resilience finally let go. He died peacefully in his sleep of unknown causes and in perfect health. I would have described his cause of death as “resilience exhaustion.” He left this verse in reflection, his variation on Tennyson’s Crossing the Bar.
Sunset and evening star,
When I put out to sea
When I go across the Bar,
I want no tears for me.
For I am very much alive,
Though I lie with unseeing eyes,
I lie not dead…
I am forever thankful that he gave me his name, his profession, and his resilience which does indeed live on.

Thomas M. Deas
1916-2020

Helena Kons, Class of 2023
After three months of excruciating hours, ailing patients that had been stuck in the hospital for weeks, and intimidating attendings who peppered us with questions...
Read More
Helena Kons, Class of 2023
After three months of excruciating hours, ailing patients that had been stuck in the hospital for weeks, and intimidating attendings who peppered us with questions out of the blue, the transition to outpatient has been smoother, calmer, and, well… Boring.
Rather than rounding on patients with appendicitis, sepsis, or aspiration pneumonia as I had during my time in the hospital, I am now doing medication reconciliation, hand holding, and counseling – So. Much. Counseling. While I’d always loved talking to patients, I find myself constantly having to redirect patients to the questions at hand to prevent them from getting sidetracked. Half the time I feel like I am learning how to be a therapist instead of a physician.
This lament is what is running through my mind as I’m sitting in my oversized white coat in my preceptor’s office, glancing absentmindedly at the ever-growing stack of papers on her desk. I’m thankful, yet again, for the surgical mask on my face that hides my occasional subtle yawn when she walks in.
“Helena, I have some bad news to share.” She is looking down at her desk, her shoulders drooping beside her. Even as someone who is training in medicine, I find her words so doctor-ish.
“Okay,” I say, a little distracted. I had been going over my to-do list in my head. Pick up the groceries on the way home, 100 more flash cards, 20 practice questions…
I take a deep breath of the stuffy office air. I have been yearning for the pace of the hospital. I missed constantly seeing patients and scrubbing into surgeries. Lately I’ve found myself agitated at the idea of spending 40 minutes with the same patient. ‘I miss just getting to do medicine all the time’
“Mr. Smith has died.”
A jolt back to reality. “That’s terrible.” I mumble. A reflexive response. But it is not before long that my mind is reeling. Mr. Smith was my panel patient—I had been assigned in my first year to follow him throughout his medical journey. I’d accompanied him to appointments, gotten to know his family, and called him regularly to check in. I was in the room for his diagnosis. I watched as he stared in disbelief upon hearing that he had metastatic lung cancer. “But I’ve quit smoking!” he’d said, “All of my last scans were normal!”
I remember his oncology appointment. I remember how rushed it all felt, and how it was to sit with his daughter in the waiting room. I remember her telling me about her son’s hobbies and her pet’s names and her father’s pride in being the patriarch of their family.
I also remember wiping away tears as I drove to my afternoon clinic. I remember missing questions in all of my other clinics because I was so distracted. I remember missing sleep as I tossed and turned, wondering how much time he might have left.
Most of all I remember feeling angry: at cigarette companies; that I was assigned to such an emotionally heavy case. Angry at myself for not being better at compartmentalizing.
This moment highlights the schism between the fantasy and the reality of being a medical student. In medical school, you inevitably become the recipient of a hefty amount of praise that you’re not entirely sure you deserve. The myth goes that patients look up to you, your friends from high school envy you, and family members gush with pride at reunions, showering you with compliments about your intelligence and dedication. In a lot of ways, you are society’s idea of perfect. You are young, successful, intelligent and hardworking – many of America’s most highly valued ideals wrapped into the two-word title — “medical student”.
Then there’s the other side of being a medical student that only you, your classmates, and your family members will understand: the constant pressure to be perfect. The pressure to make it look easy. The fear that if it’s already this hard, it will only get harder. The assignment you missed because you only got three hours of sleep for the fourth night in a row. The messy, run-down apartment with dishes that have been in the sink for God knows how long. The feeling of never having it together and never being good enough. It all serves as a constant, sobering reminder: you are anything but perfect.
As we progress through our career grappling with these personal demons, the human aspect of medicine often fades into the background. But today in my preceptor’s office, it calls me back. The first day I met Mr. Smith was perhaps the worst day of his life. I was sitting in the same seat in my preceptor’s office six months ago when she had looked up at me and said, “We have a patient coming in today, and his last CT showed metastatic cancer. We don’t know the origin of the cancer right now, but the prognosis doesn’t look good. I am referring him to oncology.”
I tensed up as I pictured myself in the room watching her give the news. I hated the thought of it, watching for the sake of learning, without having to endure the pain of lived experience. I tried to rationalize with myself. ‘Relax,’ Deep Breath. ‘You’re only a student. You’re just here to learn.’
At the time, my preceptor and I walked into the patient room together and greeted him with smiles and brightly asked him how his day was going. This time it felt wrong. There was a sucker punch coming and only we knew it.
Shortly after the niceties, my preceptor sat down at the patient level, took a breath, and said with compassion and efficiency, “We’re reviewed the results of your CT. I’m so sorry, but it looks like you have cancer. At this point we don’t know where the cancer started from, but it seems to have metastasized.”
A pause. “Okay” the Mr. Smith responds. His face remained hardened and strong, though there was no one with him for him to be strong for. He waited for us to say more.
“I’ll be referring you to an oncologist,” my preceptor continued. “It’s really important that you go to that appointment as soon as possible. I want to make sure that you aren’t delayed in treatment if that’s what you choose to do.”
I watched as his face changed from blank, to angry, to confused. My preceptor didn’t realize that the news has not yet landed.
“I don’t understand,” he responded. “I quit smoking and I had a full CT less than a year ago! And there was nothing there! Nothing!”
As I watched the scene unfold, I felt a sense of dread wash over me as if I was a small animal backed into a corner. I wanted to leave the room as fast as possible. ‘I shouldn’t be here, I shouldn’t be here.’ I kept thinking. ‘This is private. I shouldn’t just stand here and watch.’
But despite this anxiety, face-to-face with true vulnerability, I was honored to be a witness to medicine at its most human level. I stood quietly as the patriarch in front of me slowly appeared smaller, more honest, and more fragile. True imperfection. In a way, it was beautiful. Pure.
A few weeks after Mr. Smith’s diagnosis, his daughter and I sat together during his first oncology appointment. She told me her husband had recently left her and she was caring for her father and her son on her own. When they called his name for the appointment, she grabbed my hands in hers, looked at me and pleaded, “Please. None of this medical stuff makes sense to me. You understand it. You can help us.”
At the end of the day, I chose medicine. I continue to choose medicine, in the words of philosopher Emmanuel Levinas, “For others, in spite of myself, from myself.” Even when the diagnosis is beyond our control, even when following patients hurts, I choose this field because this is important work, because it needs to be done, and as I continue to learn over and over, it needs to be done with compassion. I did not change Mr. Smith’s prognosis. I did not prolong his life. But I provided a comfort to a family in struggle. I was a strong hand when someone needed strength. And in doing so, I became a part of his journey, and now he is a part of mine. That alone is a gift.

Grace Newell, Class of 2023
As I walk down the hall of the ICU toward your room, I know I am about to encounter something new. Just two days ago...
Read More
Grace Newell, Class of 2023
As I walk down the hall of the ICU toward your room, I know I am about to encounter something new. Just two days ago you were rushed into the hospital with excruciating abdominal pain: a perforated bowel, likely an adverse effect from your chemotherapy for ovarian cancer. Just two days ago you shared your story with me despite your extreme pain. Our conversation did not hide the fear in your eyes; fear of not knowing what would happen after your surgery. I shared your fear, my instincts telling me that what lay on the other side of this surgery was something no one wished for.
“Will she be okay?,” I asked your surgeon anxiously throughout your surgery, “She is only in her forties and has a husband who loves her. I hope she will be okay.”
Even as I said these words, I knew deep down inside that your chances of a long-term survival were grim. In fact, the answers to my questions lay right in front of my eyes as I looked at your pale, lifeless organs that reminded me of something I might see in an anatomy lab and not in the operating room. When we opened your abdomen, tumors throughout your entire peritoneum stared back at us. Your bowel was worse. It was so badly damaged from the chemotherapy that your surgeon described it as “frozen bowel,” unable to move or function due to the toxic medication intended to help you survive.She is only in her forties, she still has a whole life to live, I kept thinking as each minute went by and your chances of survival dwindled even more. She is younger than my mother. It was this thought that would haunt me for days to come.
Your surgeon, and then I, spoke with your dad. “I am so sorry that this has happened. Her surgeon did a good job and took the best care of your daughter that he could. I am here if you need anything, and I will be in every morning to check in on her and on you,” was all I could say.
I had no words to describe my own feelings, as I was still processing them myself. When we left your father, it was 4:00 AM and I could tell his world was flipped upside down. As we walked away to get ready for the next surgery, regret pierced my head. Did I make a mistake? Should I have stayed and sat there with him after the night he just had? But if I did that, would there be anything that I could have said to make this situation better? Frankly, I am not sure what I could or should have done in that situation, but I still think about what I might have done differently.
The next day you were awake and moderately aware of what happened the day before. Now, the fear in your eyes was met with somnolence, anger, and frustration. “How are you feeling?” I asked, even though I was afraid I already knew the answer. You shared your frustration about not knowing what would happen next. You wanted answers, but I did not have them. I felt bad I couldn’t help you in that moment. I knew you were hurting and I knew the reality of your condition was slowly sinking in. There is so much I wish I would have said to comfort you in this time, but I couldn’t find the right words to help. “I will make sure all your questions get answered, and if there is anything else I can do to help please let me know. I am here for you and as a medical student it is my job to be an advocate for you,” I explained. Then I left your room not knowing that was the last thing I would say to you before you were sedated, intubated, and transferred to the ICU.
It all happened so quickly. One day I was talking to you and you were responding. The next thing I know I was standing next to you and I was still talking, but you couldn’t respond. It felt unusual for me to talk to someone whom I knew would not respond, but it felt necessary. “Good morning,” I would begin, “It’s Grace the medical student, and I am here to check in to see how you are doing.” Clearly she is not doing well, I would think to myself. However, I continued, “I am going to perform a physical exam and I will walk you through what I am doing.” I listened to your heart and lungs. I examined your dressing that was covering the opening to your abdomen that was never closed. I looked at your ileostomy and documented my findings. At this moment I became haunted again by my recurrent thought: She is younger than my mother. Then, I looked at your face where I once saw fear, anger, and frustration, but now saw peace and tranquility. I held your hand and said out loud, “It was nice seeing you again this morning, I will see you again tomorrow.”
I looked at your father, who responded, “Thank you for coming to see her today. I am glad she is no longer in pain.” I let him know I was here if he needed anything and the nurses were just outside the door. I left your room, just two days after meeting you thinking to myself, I hope to see her again tomorrow.
The next morning you were gone. You passed quietly in your sleep with your father right next to you the entire time. You were younger than my mother, you still had so much life to live, and I continue to wonder if there was something more I could have said to comfort you in your last days. It is funny how much communication can change in just a few days. One day you and I were able to have a conversation, and the next day I find myself talking to someone who I knew was never going to talk back.
_______________________________________________________________________
**Photograph taken by author, Grace Newell, with a black and white film camera then developed in a darkroom.
“To me the leaf reminds me of what we saw during her surgery. Something fragile and lifeless, yet something that was so beautiful that was part of something bigger than the damaged spots that lay on the dying leaf. Just like the tumors taking over her body when her beauty and strength overpowered what she was battling with.”
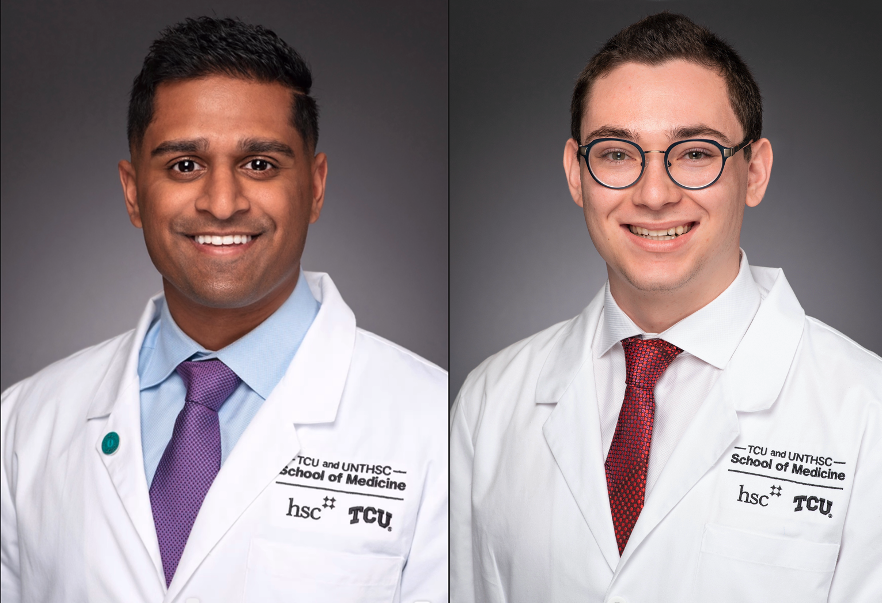
Arsalan Ali, Class of 2024 and Benjamin Jacobs, Class of 2024
Arsalan Ali “I feel very alone.” After several months of being completely online for medical school due to the pandemic, my life started to feel...
Read More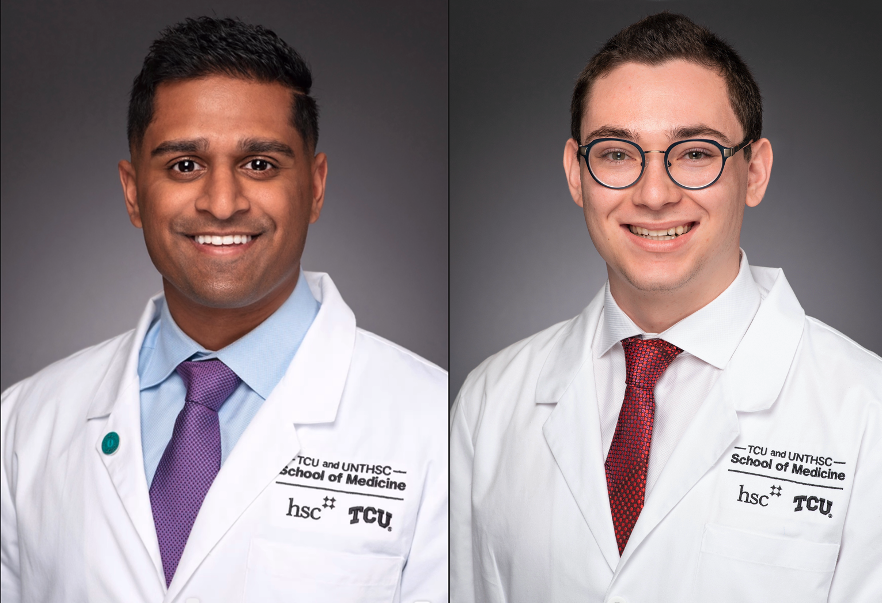
Arsalan Ali, Class of 2024 and Benjamin Jacobs, Class of 2024
Arsalan Ali
“I feel very alone.”
After several months of being completely online for medical school due to the pandemic, my life started to feel like a never-ending loop within my one-bedroom apartment. Wake up at the same time, turn on my computer, attend class from a small box, eat lunch, study at the same desk for another few hours, eat dinner, and repeat.
The days of the week began to blur together and the boundary between school and home collapsed. I was on autopilot, and I was just going through each day feeling dissociated from my own body, mind, and emotions. I put on a fake smile around others and hoped they would not intuit how I really felt; alone, trapped, defeated, and frustrated. I created a facade subconsciously to show others that I have what it takes to be in medical school, and I am not easily broken. As a first-generation student, I realized at an early age I have to be grateful for the opportunities presented to me. I have never felt empowered to the right to complain as my parents have sacrificed so much for me to be here. Growing up, my dad continuously reinforced to me, “get an education so that you don’t have to work as hard as me.” My dad was the son of a farmer in India. It was deemed that his future would also make him a farmer, but my dad hoped for a future where he could provide his children with a proper education. When the opportunity came to come to America, my dad seized the chance. He came with no education beyond middle school and little to no English.
For over 15 years, my dad worked multiple jobs at the same time, but his mind was just focused on his children to get an education. Despite our financial situation, my parents ensured that I had school supplies and access to tutoring if needed. As I would moan and groan about school, he constantly insisted that education is the key to a better life. Soon enough, his constant reminders and motivation kept me focused on school and to always try my best under any circumstances. Although my background has helped me get far in life, ironically, it was my biggest pitfall during the pandemic.
When I was accepted a position at TCU and UNTHSC School of Medicine in May 2020, it was a dream come true. The years of studying and countless hours spent on MCAT preparation were finally going to be worth it. Like many students starting a new chapter of their life, I could not help but daydream about medical school. I was excited and anxious to move away from my hometown for the first time and meet my classmates. I heard from many mentors that although medical school is challenging, it was the best time of their lives. It was a place where they felt challenged every day and met their lifelong friends. I know now that it was naive to have this “perfect” vision during COVID-19. I was overly optimistic that the pandemic will vanish by the time I started school in July. November: “The cases are still rising and we are unsure when we will be back in person,” said the official message from the school of medicine. At this point, the zoom fatigue was in full effect, and I was a prisoner in my own apartment. Confined to a small space, making laps around the kitchen counter to stretch my legs, and feeling more alone as time passed. I am an avid believer that you learn medicine in a community, and in a virtual world it becomes easy to dissociate yourself with just a click of a button. I was timid to share this feeling with the rest of my classmates as I did not have a close bond with many of them.
It was not until our school did a class survey which revealed that on average our class does not feel connected to each other, however, 65% of us “extremely” wanted to make this connection. For the first time, I felt like I was not alone, but in fact there were nearly 60 other students who felt just like me. As we began to have more in person interactions, our class bonded over this similar feeling. We all wanted to feel a sense of belonging and develop deep connections. After a year of being restricted to a small video square, our class is finally getting the opportunity to finish our phase 1 curriculum in person. It almost seems surreal that after months I am going to get a glimpse of that “perfect” vision of medical school. The year was relentless, and I had to be the same. It was a ‘year of missing’ in medical school- missing traditions and making memories, missing home, missing the feeling of being surrounded by your classmates, and missing the feeling of wellbeing and joy. All of these are important for student life balance, and as I reflect on this year, I have grown so much as a person and a student. The pandemic has shown me that loneliness is real and human connection is crucial for wellbeing. I am ready to continue being relentless and grateful for everything that comes my way as I begin my second year of medical school with the #strong60.
Benjamin Jacobs
Resilience is defined as “the capacity to recover quickly from difficulties; toughness.”
All my life I had to be resilient. When I was growing up, my family moved constantly– so much so that by the time I graduated high school, I had attended eight different schools in multiple states. The longest run I ever had in a single school growing up was three years. The hardest part about being the “new kid” all the time was making friends. Making friends was exhausting because I felt like I was intruding on friend groups that had been formed for years. In the back of my mind, I knew that when I moved to a new school it was only a matter of time before my family would move again. This feeling made me timid and apprehensive to get close to people because I didn’t want to start a friendship, get close to someone, and have to deal with the sadness of leaving them.
When I graduated high school, I knew college would be yet again another test of my resilience. For college, I went to the University of South Dakota (USD) in Vermillion- a small town of 10,000. The four years I spent in Vermillion was the longest consecutive amount of time I had ever spent in one community. There is something special about being in a small community- everyone leans on each other for support. This connection and consistency was something I had always wanted but never had. My experience at USD made me realize that for medical school, I wanted to go to a program with a small class size-where everyone leaned on one another.
When I received my acceptance call from the TCU and UNTHSC School of Medicine on November 1st, 2019, it was the best day of my life, filled with a rush of conflicting emotions: excitement, fear, anxiety. I knew that medical school would be a big transition and perhaps the biggest test of my resilience yet. When the COVID-19 pandemic began shutting everything down in March 2020, I remained optimistic: “Surely everything will be under control by the time I start medical school in July…Right?”
Flash forward: a majority of my first year of medical school was completed remotely from my 15-inch laptop screen at my apartment, guided by a small path through my apartment. Every day I would wake up, walk two feet over to my desk, sit there for hours, and when it was time to go to sleep, I would walk two feet to my bed. Rinse and repeat. My routine was identical regardless of the day of the week; the days began to all blend together.
When my friends and family would ask how medical school was going, I put on a happy face and told them it was going great. I exaggerated how much my classmates and I were interacting despite the pandemic and downright lied at times about our classes being in person. Why? I think this facade I was putting up to my family and friends served as a coping mechanism for me. I would tell them about how my classmates and I went exploring the town (when we really just talked in the parking lot) or how clinical skills in person was nerve-wracking but exciting (when it was actually online). I was living vicariously through the stories I was telling my family and friends.
Being remote made me realize how much I craved physical touch. Something as trivial as a hug, handshake, or even a fist bump between two people just feels human– this was one element that made me feel so disconnected and alone over the past year. Even when we did have class in person and I was finally able to put my hands on a patient, we each had masks, goggles, gloves, and face shields. It felt forced and artificial. Ironically, I realized at some point that the closest I got to putting my hands on a patient my first year were the dozens of prostate exams I was taught to give by my preceptor in clinic. How odd is it that I couldn’t shake a patient’s hand, but had to perform an invasive exam like this one…
But, I wasn’t alone in this feeling. In the clips of speaking with my classmates six feet apart in parking lots or in masks or through screens, we all felt this irony: that some of our most consistent forms of touch have been through our training to perform some invasive and uncomfortable exams on patients.
This past year was not easy, but it taught me that whatever situation you are going through, no matter how difficult it may seem, someone else is going through it too. That is what unites us.

Toni Igbokidi, Class of 2024
Inside rooms where spirit is tethered to time Lie incubators — warm and full of gab, frisk with Glimmer and giddy — defiant souls of...
Read More
Toni Igbokidi, Class of 2024
Inside rooms where spirit is tethered to time Lie incubators — warm and full of gab, frisk with Glimmer and giddy — defiant souls of lesser green grass Naive whetted scalpels and abandoned bellies Naive to Caesarean sutures, iron-bounded one too few Naive of dread towards strange fruit and hooded men — white She stands tall in the wilderness of trees born steel and nitrile stockings Majestic like high-jumping gazelles, where no heights are Greater than post-partum hypertension or gestational diabetes Her father tells her that she is Brown Sugar in a white coat And that her smile creates Rainbows out of raindrops sphering over horizons obscured Epidurals pierce through spine colored with Melanin and scar tissue left by ancestral lashes Nourishment — discovered amongst the juxtaposition of her mother’s tears and prayers Outgrowths of bantu knots and unwavering resolve Reveal that she is standing on the precipice of her own presence Giving birth to a new era of woman

Juhi Shah, Class of 2023
In the webcomic The Oatmeal, illustrator Matthew Inman tackles the backfire effect. He goes on to discuss how the part of one's brain called amygdala "makes...
Read More
Juhi Shah, Class of 2023
In the webcomic The Oatmeal, illustrator Matthew Inman tackles the backfire effect. He goes on to discuss how the part of one’s brain called amygdala “makes us biologically wired to react to threatening information the same way we’d react to being attacked by a predator.”1 Inman’s comic was a popular statement in anticipation for the 2016 election and presently remains relevant due to its wry humor and ongoing significance on why people are so resistant to hearing contradictory facts. However, many political scientists found it hard to replicate as a large-scale peer-reviewed study could not reproduce the findings.2 I felt myself backfiring from reading the backfire effect. This phenomenon is the epitome of how debates begin, of how medical ethics are handled, of how scientific research is initiated.
The motivated reasoning and confirmation bias that Inman discusses in the backfire effect can be manipulated in medicine, similar to the “truthiness” model. Dr. Jeffrey Matthew from the University of Wisconsin adopts Stephen Colbert’s illustration of the “truthiness” model as “Truth that comes from the gut, not the book.”3 The backfire effect and the “truthiness” model are some of the reasons as to why trusting the knowledge that professors, peers, or anyone else impart is so difficult for me. From one angle, I could see the controversial information that was taught to me as something that is just testing the resistance in my amygdala.
I observed the bleak reality of clinical based medicine as something that has been anecdotally passed down to form “truthiness” yet have no evidence-based methodology. For example, we were taught the five most common causes of postoperative fever with one of the causes being atelectasis (partial or complete collapse of lung). However, the relationship between atelectasis and postoperative fever is unsupported. This ongoing tug-of-war between what is factual and what is practiced is the foundation of curiosity in medicine. It’s why I was interested in this profession in the first place.
I was looking for answers. I did not want to look for them in books. That is why I consider our clinical rotations, known as the Longitudinal Integrated Clerkship (LIC) a perfect program for students like myself. TCU & UNTHSC School of Medicine’s LIC incorporates multiple specialties in one longitudinal rotation for approximately 40 weeks. This type of integrated learning allows us to test controversial information such as indication for which diabetes medication to prescribe in the various specialties. These experiences allow us to decide upon our self if these “clinical pearls” are a part of the backfire phenomenon or a form of “truthiness”.
Several patients one day presented with evidence-based urgency hypertension, something I had recently read about but had not yet seen in my patients. These patients had blood pressures well over 180/100 such as 191/106 and 185/103, whereas normal blood pressure is 140/90. Proper protocol from my notes would suggest “oral antihypertensive agents, including β-blockers, angiotensin-converting-enzyme (ACE) inhibitors, or calcium channel blockers.”4 Proper protocol in my clinic: perform the HPI for the patients concerns and not address the hypertension. Talk about backfire.
I began to question if evidence-based medicine is preferential over clinical based medicine. I asked my internal medicine preceptor her thoughts on the difference between clinical based and evidence-based medicine in this scenario and she stated “What evidence-based medication does not always take into consideration are the social factors such as patient compliance and adherence along with socioeconomic disadvantages. When those factors arise, that is when clinical based medicine becomes preferential to evidence-based medicine.
This is where I had to start learning the difference between clinical based practice and academic based practice. I found several articles on UpToDate that both supported and contradicted the clinical based practice in measuring high blood pressure in the clinic. My realization from this search was exactly what Dr. Jeffrey Matthews touched on in his lecture: “evidence is elusive.” Proper protocol depends on what year of research does the physician base their protocol on, the type of medicine (clinical or evidence-based) the physician practices, and just the physician her/himself. Now that I have learned, seen, and practiced the difference, this is a lesson that will never be forgotten.
By any circumstance, this narrative piece is not me passing judgement. This reflection is about me ultimately realizing how medicine is fluid with waves of preference in evidence-based medicine or clinical based medicine. As a naïve medical student, I supposed the two would be one. Oh, understanding that the two types of medicine are rarely unified backfired on me- and my amygdala, the emotional cortex that hosts our core beliefs!
1 Inman, Matthew. “You’Re Not Going to Believe What I’m about to Tell You .” Comic strip. The Oatmeal, 2016. https://theoatmeal.com/comics/believe.
2 Haglin, Kathryn. “The Limitations of the Backfire Effect.” Research & Politics 4, no. 3 (2017): 205316801771654. https://doi.org/10.1177/2053168017716547.
3 Truth and Truthiness in Surgery . Truth and Truthiness in Surgery , 2016. https://youtu.be/swYKy_u3If0.
4 “Emergent Hypertension.” USMLE-Rx. Accessed June 2, 2021. https://usmle-rx.scholarrx.com/rx-bricks/brick/CP_CAR0087.

Lauren Moore, Class of 2024
I named you “Babar.” A familiar fixture on my face so permanent Bloodied blisters bloomed where skin and plastic met. The soft space between lip and nose wrinkled from weeks...
Read More
Lauren Moore, Class of 2024
I named you “Babar.” A familiar fixture on my face so permanent Bloodied blisters bloomed where skin and plastic met. The soft space between lip and nose wrinkled from weeks of crusted snot and Surgical tape. Our initial introduction was a bitter omen For the month that lay ahead. And I, a nonconsenting participant, fought wildly Against the pain while attempts to unify us failed— Repeatedly. One Two, three, Four, five tries before soothing voices whispered “swallow.” You were there stroking my gag reflex as Blood and tears leaked down my sweat-stained face. Just you and me, Babar. My parents fled the room To escape the attack on my nasal cavity. But they would come to know you too. Our union, My elephant appendage, would be the center of the circus And a brazen burden on all. For weeks noxious green flowed freely through you— A fast track from stomach to the external world. Internal physiology exhibited for all to gawk, an intimate connection Requiring diligent hands to sustain filling demands. Clamp, empty, connect, repeat. I pleaded for water while you sucked me dry. An assault of daily depravity and cruel balance of power yet— I grew to love you. Together we weathered Surgeries, sepsis, starvation. 20 pounds we lost together Catheters, a central line, and drains. A comradery visible yet unfelt among observers For you both delivered and understood my pain. But then ice chips replaced cracked lips As food for blood was swapped for solids, And I was left abandoned in your wake. Freedom was redefined by your depleting grasp And I forgot how to receive. I dreamt of liberation, but fullness led to rejection. Offerings of cotton candy ice cream, confetti sprinkles, And stinging bile swirled in a bedpan. Days spent begging for relief replaced with hopes of emptiness— A mouthwatering sickness of conflicting desires. Was it the gift of life or hefty price for outsmarting death? A searing throat from eating then retching. Retching then eating. Fond memories of us now fleeting.

Dilan S. Shah, Class of 2023
She was my first real patient. Before the pandemic, I regularly saw her at my family medicine clerkship for routine follow-ups. Always accompanied by her...
Read More
Dilan S. Shah, Class of 2023
She was my first real patient. Before the pandemic, I regularly saw her at my family medicine clerkship for routine follow-ups. Always accompanied by her adoring daughter and designated caretaker, they would teasingly call me “baby-doc” as I fumbled with my stethoscope.
Now, almost a year later, I was holding her small bowel between my gloved fingers under the bright lights of the OR. As I ran my hand down the loops of intestine, I felt crunching– “I think I feel pneumatosis intestinalis,” I said to the surgeon. He met my hand at its place on her bowel and felt. “The kid is good,” he said to the scrub nurse, “nice catch!” Oh the validation of a correct diagnosis. Though eager excitement quickly made way for dread. I knew what this meant. Her intestines were dying, she was at the end of the road.
We met again 7 days ago in the emergency room when I was on-call. Fear of coming to a hospital full of COVID left her in agony for months as she ignored early signs of her dying organs. Serendipity or fate, when she did finally come for help, I was there.
I was with her in the hospital room, where she laid helpless, vulnerable and scared. I was with her in the OR where she laid open, vulnerable and exposed. Balancing the duality of humanity and science, I held her daughter’s hand after each surgery and translated the surgeon’s medical jargon. I was the last person she talked to, giving soothing words as the anesthesiologist put her under, never to awaken again.
Her final days were spent unconscious and intubated in the ICU. Her daughter was by her side every day, for as many hours as COVID policy allowed. Between patients, I would go down and visit them. We would sit and I would listen to her daughter tell stories of her kind and quick-witted mother.
On the final day of my Surgery rotation, and what I would later discover would be her final day of life, I wrote her family a letter. Simply to share how grateful I was to have learned from their mother’s case, wishing them peace in the soon-to-be passing, and offering whatever soliloquy of comfort I could. It was a simple gesture, one that I figured would be met with a few moments of gratitude and then slip to the back of their consciousness and forgotten in grief. Months later, her daughter would reach out to me to share how impactful that simple gesture was for her family’s coping.
I chose medicine, because in no other field are you stretched to be both so technically proficient and emotionally vulnerable. The science of medicine is constantly infused with the raw emotion and heavy responsibility of having a human life in your hands. To have such privilege is a beautiful burden.

Caden D. Duffy, Class of 2024
I walked into the patient’s room and saw my sister. At least, Mary* could have been my sister for her age and complexion seemed to...
Read More
Caden D. Duffy, Class of 2024
I walked into the patient’s room and saw my sister. At least, Mary* could have been my sister for her age and complexion seemed to match. As I opened my mouth to speak, her shaking hands, thick palpable nervousness, and a downwards stare portrayed an individual uncomfortable and unaccustomed to a physician’s office. I greeted her with a smile, stating my name, position, and purpose. Just as I had with the patients before her, my first question was to ask why she had come in. The words—“I’ve been feeling depressed”—were quickly and quietly spoken.
I witnessed Mary’s familiar face lower to the floor as her quiet, delicate nature came to light. I felt a reverence for her feelings of grief, a scene that might quickly be compromised due to my inexperience. It took a few moments, but she gradually warmed up to our discussion as I centered the interview around her journey to the office. We talked about her mother’s supportive and guiding influence which had led her to request the visit. We discussed the coping mechanisms she was trying, including an increased reliance on marijuana, which had proven unsuccessful in warding off feelings of self-doubt. I reassured her that the attending physician would provide excellent care, good enough that I would recommend him to my own sister. A vivid image of my sister passed through my mind. I could see her, or them. My conversation with Mary felt familiar.
Despite that I had never worked with a patient challenged by mental health concerns, my confidence in understanding Mary climbed as I completed her interview. Perhaps due to her semblance to my sister, I left the room with what I felt to be a complete picture of her condition. As I began my oral presentation to my preceptor, I boldly told him of her one-year history of feeling depressed. I described in detail her symptoms, including nausea and vomiting, which I proudly deduced had stemmed from her use of marijuana.
The seasoned physician listened patiently and then paused for a moment. “Did you ask Mary if she’s ever considered killing herself?” he asked. I stared back at him. I was tempted to try and rationalize why I had not, especially with all of the other important history items that I had obtained. “No,” I frankly replied back, somewhat embarrassed by overlooking what he knew was a key part of her history. Like an expanded balloon experiencing an air leak, I felt the common deflation of an overly confident medical student. I discreetly tried to cloak the puncture.
Why hadn’t I asked? Without meaning to, I thought about how my sister would never do something to hurt herself. Even with family, suicidal ideation can be a sensitive subject to address. I didn’t want to intensify my discussion with Mary, especially since she had already extended herself in discussing her drug use. Mary was vulnerable in coming alone to a new provider visit. I would need appropriate justification to ask a question like that. If she did struggle with suicidal thoughts, what would I have to do with that knowledge?
As I contemplated these questions, the attending told me about selective serotonin reuptake inhibitors, or SSRIs. They are one of the most commonly prescribed antidepressants. Citalopram, or Celexa, works very well to treat patients who are experiencing depression. However, there is an FDA black box warning prominently displayed on the side of the medication. This warns of the possible increase in suicidal thoughts or actions in some young adults at the initiation of treatment. For these patients, prior suicidal ideation is further investigated with extreme precaution prior to prescribing the medication. If these thoughts are already present, alternatives are further considered. Completely unaware, I had left Mary’s room without a vitally important aspect of her history. Although the medication could improve how she was feeling, giving Mary this antidepressant could contribute to a negative and permanent change to her life.
We returned to Mary’s room and learned that my preceptor’s inquiry was especially important in our visit. I observed the connection that he made with Mary, gathering key information and using her responses to create a treatment plan. We discussed our options and decided to prescribe Mary a different medication. Although the conversation was difficult and personal for Mary, my preceptor’s kind but direct questioning inspired me to better obtain a more complete medical history out of each of my patients.
Someday I may encounter a sister, brother, friend or neighbor sitting in the corner of my examination room. In spite of the familiarity, I need to work towards gaining an unbiased and more complete understanding of the information which could impact their health. Like with Mary, I look forward to understanding who my future patients are, and how best to treat them, through asking the right questions. This will probably not be the last time I walk into a room, and see my sister.
*The patient’s name has been changed to ensure privacy.
by Emma DiFiore, Class of 2024
Maybe it is the fact that the clinic I have been placed in as a first-year medical student is primarily patients aged 65 and up,...
Read More
by Emma DiFiore, Class of 2024
Maybe it is the fact that the clinic I have been placed in as a first-year medical student is primarily patients aged 65 and up, or maybe it is the tremendous amount of death we have all faced this year amidst the COVID-19 pandemic, but lately I’ve been pondering what it means to experience death in the field of medicine.
Recently, I had a discussion about death with my clinical skills preceptor, Dr. Ashley Huddleston. She started her career in emergency medicine, constantly in the face of death. She oftentimes only knew these patients as “ill” or “dying” as opposed to in primary care, where patients are seen in all facets of life. Dr. Huddleston has since changed fields of medicine to wound care and hyperbaric medicine: rehabilitation. Now, she gets to watch as her patients experience life. She gets to form relationships with them, often seeing them weekly. Yet, interestingly, she stated that this now makes death more difficult to swallow when it does come. These long-term relationships in outpatient medical care become so pronounced, as opposed to the sometimes unfamiliar nature of relationships in inpatient care. These humans are no longer strangers, but companions.
I cannot predict how I will face death as a medical professional or even as a human. But I do know I want it to be as intimate and raw as the day I had first experienced a healthcare-related loss. I was interning at an outpatient addiction treatment center that summer. It was unexpected. It was angering. It was reality. Here is an excerpt of my writing based on that day:
“A typical Monday morning as an intern at an intensive outpatient addiction treatment center is brimming with positive energy and new beginnings. Pulling up to the office, I would see the clients chatting and laughing on the front porch. Their communal cigarette smoke mingled with the sweet scent of gardenias in the summer air. Inside the center, which resembles a quaint pink cottage, the therapist, the medical director, and a pot of freshly brewed coffee would joyfully greet me. Monday mornings felt like sobriety was at our clients’ fingertips – until it wasn’t.
On July 5th, Monday morning felt dark. The porch was empty and humorless. Its usual inhabitants sat confused and quiet inside the group therapy room. The staff’s office doors remained shut. No one there to greet me. No freshly brewed coffee. Minutes felt like hours as we waited. Eyes scanned the room to see who was there and who was not. With heads bowed, the staff entered and took their seats. The silence was finally broken: ‘Joe; had overdosed and passed away. Joe, the one who everyone in the program looked up to, who was thought to be the last person this would happen to. Addiction had won, and its triumph rang loud in the silence of the room.
I have regularly come back to that somber July Fifth when Joe lost his fight. That day,
there was a sense of quiet perseverance. Reflecting back, I realize how difficult it was to retain such fortitude amidst tragedy. Nonetheless, each one of us left holding our heads a little higher — the patients, the therapists, the physicians, and me. The patients persisted in their fight for sobriety. The therapists and physicians persisted in their inclination to treat those suffering. I, aching for that same inclination, persisted in my pursuit of medicine. In that vulnerable moment, gripping each other’s shaking hands and wiping our weeping eyes, we were able to bridge the gap between patient, intern, and provider. There was a genuine camaraderie that day which left us all at ease.”
This memory is frozen solid within me. And it was what pushed me closer to medicine. In fact, without this experience, as tragic as it was, I do not believe I would be where I am today. It is not that it motivated me, it is that it matured me. It revealed to me the realities of medicine, while erasing the previously glorified view I had of medicine as simply healing.
Will this experience prepare me for future confrontations with death? Possibly. I just hope whenever death comes, I am surrounded by people in the most humanely raw way possible. No hierarchical labels of physician, resident, student, or patient — just fresh human emotions, compassion, and perseverance.

Do you have a HuMed inspired photography series you'd like to submit? Visit our submission page to send us your ideas or connect with Erin...
View PhotosDo you have a HuMed inspired photography series you’d like to submit? Visit our submission page to send us your ideas or connect with Erin Nelson, PsyD to discuss.
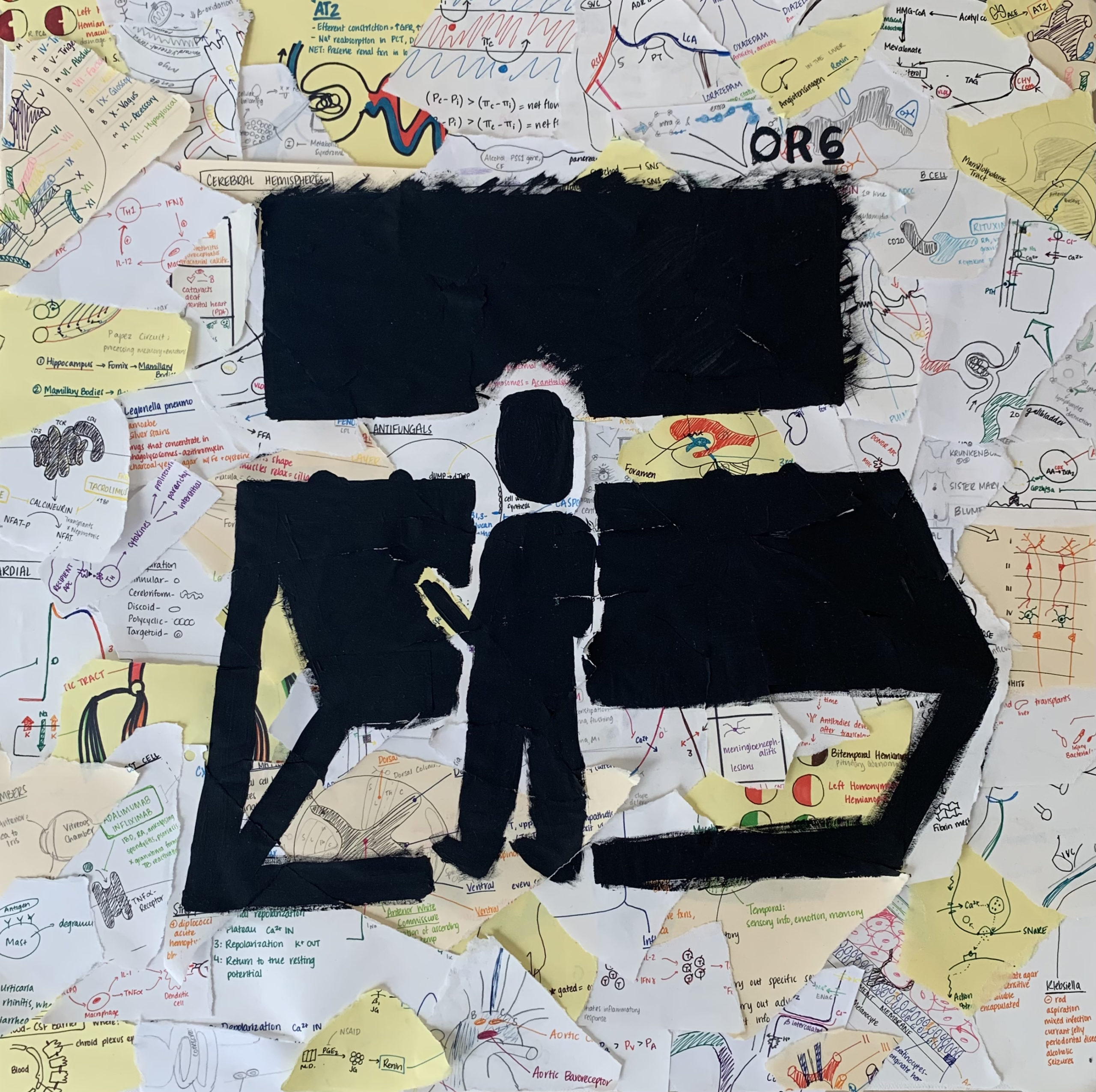
Sarah Lyon, Class of 2023
paper and ink, tape, and acrylic paint on canvas A Medical Student’s first time scrubbing into the OR. Snippets of everything they learned during didactics...
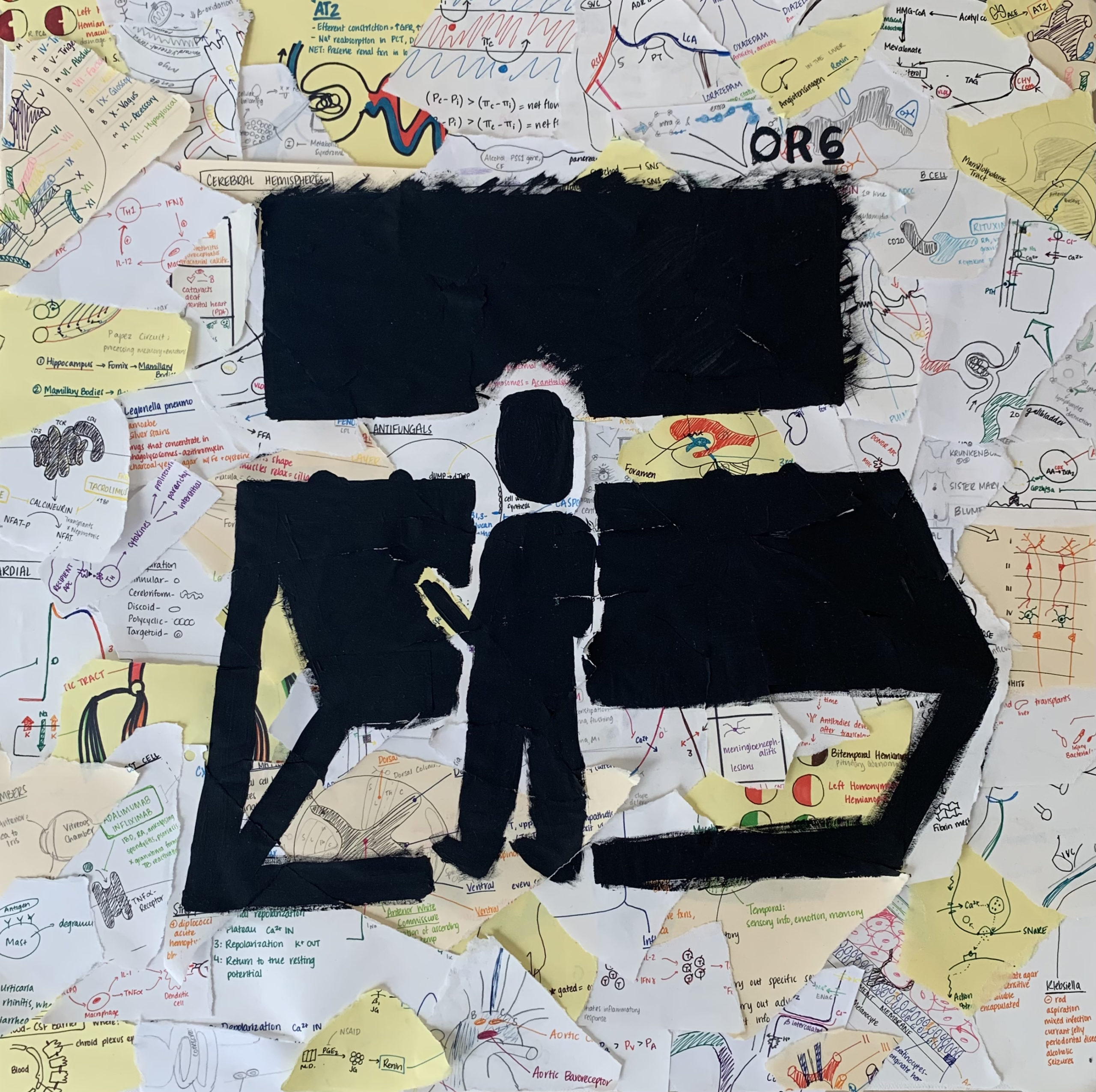
Sarah Lyon, Class of 2023
paper and ink, tape, and acrylic paint on canvas
A Medical Student’s first time scrubbing into the OR. Snippets of everything they learned during didactics flashing in their mind. Looking into the unknown darkness of OR 6, unsure of what is to come. Will they be prepared and competent enough to provide exceptional, empathetic patient care?

Kavneet Kaur, Class of 2023
Character Description Kavneet: A naïve 3rd year medical student working a shift in a rural Emergency Department at the time of yet another COVID surge....

Kavneet Kaur, Class of 2023
Character Description
Kavneet: A naïve 3rd year medical student working a shift in a rural Emergency Department at the time of yet another COVID surge. Must work shifts for 28 out of 31 days this month. Tired, but ready to work and take on a challenge. Always hopes for the best and tries the see the good in a bad situation.
Scene: It is month 8 of 10 of my Emergency Medicine rotation and delta variant reared its ugly head.
====================================================================
[Cruising down the highway at the crack of dawn with the window rolled down, I let the cool, crisp air wake me up. The radio is screaming on repeat: “The death toll from COVID-19 is increasing day by day… Delta variant seems to have world leaders worried of yet another spike in cases”. As I pull into the parking lot, two deer cross in front of me near the entrance of the hospital. You don’t get that in the city.]
Hour 0
KAVNEET: “How is this shit still going on?” I grumble to myself as I walk over to greet my attending in the breakroom. I notice the tracker board with the list of current patients… just when I thought I was going to have a ‘Q word’ day.
“Q word” means “quiet”, but you don’t dare say that word in the ED unless you want all your staff cursing you out an hour later while being knee deep in patients that decided to take a trip to your emergency resort.
I overhear the overnight attending pass off a patient to my attending physician, who in disbelief remarked “This was the same patient I had on shift two days ago.” The patient is COVID positive and is currently waiting to be transferred to another facility for more intensive care, but no hospital nearby is accepting patients.
They have now been in isolation for more than 72 hours. Imagine a 6-foot by 6-foot room with white walls and no windows. No human contact outside of nurses coming in to give you meds or adjusting ventilator settings. Sedated. Looking more machine than human. Listening to the music of the vital monitor beeping similarly to a ticking clock, amid chaos happening in the room to the left and to the right of you. Lifeless.
It is quite literally the closest thing to solitary confinement without being imprisoned.
My trance breaks as we rush through the remainder of the patient list. I notice there are others waiting more than 40 hours needing to be admitted to the second floor for inpatient care.
Here’s the thing that the public tends to forget- there are still a portion admitted patients in need of critical care, who do not have COVID. This could be your grandfather having his first heart attack, your significant other that just got into a car crash or is having a miscarriage, or your child that is about to slip into a diabetic coma.
And the fact of the matter is that there may not be a place to put them or stabilize them. Even if we can, they are still left waiting for another hospital to “accept” them to get the care that they need.
Why does someone need to be interviewed to see if they are sick enough to be treated? How does that make sense?
Hour 2
KAVNEET: More patients are checking in. COVID patients get priority, especially if they have a below desired oxygen level. In other words, “priority” means you can be put in a room with an actual door that closes. What do we do when those rooms run out you ask? I pray to God. You pray to whatever Higher Power you believe in or just hope for some good vibes. “We have NO rooms open for COVID patients!” I hear the charge nurse scream as if it was not obvious. Though by the look in her eyes, more a scream of frustration than one to state facts. Let those prayers begin. We now have no option but to fill in these makeshift “rooms” with possible COVID patients. Picture a room divided into smaller sections by a shower curtain instead of an actual door. I try to justify it to myself as, “well, it’s not like there is any other place we can put them, and we can’t just stop seeing patients.”
Hour 3
KAVNEET: I do the best I can to help my attending and the staff see patients. At one point, I go to the front to help triage patients, some of whom had now been waiting for at least an hour. Our triage room is quite literally the size of a closet, so you can imagine how this was about to go.
With my head held high, a N95, surgical mask, and face shield, I march into the lobby and scream the first patient’s name to bring them into our broom closet. Yes, scream…it is that chaotic. I ask what brought them to our ED today. Cough, fever, shortness of breath? What a shocker.
“Have you been vaccinated?” I question with skepticism. No? Surprise, surprise. I proceed to get the vitals. Blood pressure 142/94… eh, won’t kill you, temperature 99.8… low-grade fever, heart rate 104… tachycardic, oxygen saturation 92… mildly hypoxic. Yep, this is to be expected. Ok now to swab for COVID.
Like clockwork, now onto the next one.
Hour 3.5
KAVNEET: We officially maxed out on the makeshift rooms, but we still have a lobby full of unseen patients. “What can we do? I understand we don’t have any space to put them, but we can’t turn them away,” my attending physician shouts through his N95 to the charge nurse as he rushes to check on a critical patient that just came in with low oxygen saturation. “PAGE RRT STAT”.
34-year-old female, with oxygen saturation in the 50s.
As my attending and others work to assess the gravity of the situation, the rest of us manage to add two gurneys and a chair… three extra spaces in the hallway of our small boondocks ED. If a code blue walks in through the door right now, we would literally be doing it in the ambulance bay outside of the hospital. Totally code compliant.
I rush back to the critical patient that was brought in. Everything and everyone moved like an assembly line. Prepare the meds, sedate, paralyze, intubate, get out. I open her chart and glance through it. She is a healthy young woman without any health conditions. She has had COVID-like symptoms for 2 days and began to develop shortness of breath overnight. So why is she this bad? Something is not adding up…Vaccination status? Unvaccinated.
As we exit the room, the front door almost knocks me down as the medical director of the Emergency Department darts in through the door. Before I can process, monitors start going off. BEEP BEEP BEEP! The patient that we just intubated… a bunch of staff rush in and one of the nurses’ pages RRT again. Oxygen saturation is 70. I stand outside the room as I see the panic in everyone’s eyes. There’s simply no time for this right now.
My attention diverts behind me as I overhear the charge nurse and medical director calling hospitals from DFW to College Station to find beds so they can move our current patients out to add new ones to the trenches. The medical director even made a personal call to the CMO of the hospital system. Little did I know that in the last several hours, we were still getting calls from the transfer center to accept patients from Kansas.
Hello? What happened to the entire state of Oklahoma?
Hours 4.5 to 9
KAVNEET: We come up with a plan to open a currently unused space on the second floor to put some non-COVID, lower acuity patients. One of the nurses told me this is the first time since the pandemic began 1.5 years ago this was being done. And for the first time since beginning my shift, I force myself to find a moment to stop and take in what is going on around me.
Do you think if an unvaccinated person saw face to face what it looks like to have more than a “COVID cold”, they would change their mind about getting vaccinated?
I often think about that young lady on the vent. If she made it off, her life will never be the same.
On a systemic note, I’m still trying to grasp how we got here? I see nurses, techs, RTs, pharmacists, radiology techs, and physicians running around the hospital trying to do the best they can, trying to solve problems that were created by this system, trying to juggle tasks out of the scope of their practice on top of their normal duties because there is no one else there to do it. I am appreciative of how hard each team member worked in our small ED that day. They are the true embodiment of perseverance and fight.
On top of dealing with a public health crisis, the unfortunate reality of working in a small ED such as this one is that patients are at risk of dying, simply because they cannot get to another facility for more intensive care. Bigger city hospitals will not accept more patients because they are also being bombarded with COVID, and statistics show that most of these patients are also unvaccinated. Even then, at least the bigger hospitals are equipped with resources and specialists to handle the surplus. To put it into perspective how smaller, boondocks EDs are affected, if you are unfortunate enough to come on the wrong day, your options are to talk to someone through an iPad or get transferred to another facility that has someone physically there to take over your care. Often, it’s the latter and we are 40 minutes from the nearest big city hospital.
If being vaccinated means less stories like what you just heard, less burnout for the people who are tirelessly and endlessly taking care of you and your loved ones, less loss of the ones you hold close to you and heck, maybe even you yourself. The question I then pose to you is: If you do not have a legitimate medical reason to not get vaccinated, what is the hesitation to get the vaccine? Whether you are pro-vax or vaccine hesitant, we can all agree that we are mentally and physically tired of this and want life to go back to “what it used to be”.
====================================================================
**This piece was a finalist for the inaugural production of Stethoscope Stage

Shanice Cox
Written & Performed by Shanice Cox [audio m4a="https://mdschool.tcu.edu/wp-content/uploads/2022/05/Take-a-moment….m4a"][/audio] Take a Moment Chapter I: Obstetrics and Gynecology Take a moment... to breathe Take a moment...to...

Shanice Cox
Written & Performed by Shanice Cox
Take a Moment
Chapter I: Obstetrics and Gynecology
Take a moment… to breathe
Take a moment…to seize…this moment that sits before you
Take a moment… to see,
beyond the gown, the drape, or the anatomy
Take a moment… to listen to the history,
To the crackles in her speech, to her hesitation,
To the hum in her pause, to her tone’s vibration,
Take a moment… to view
What it is that lies in front of you
As her hand is carefully positioned behind her head,
And the gown is respectfully placed,
while ribbons gently touch the side of the bed,
and the slight embarrassed flush of her face
Take a moment…to view
the contour of her breast
Clockwise and counter
view symmetry, asymmetry,
are you still there?
Or has she become a mindless exercise of your checklist,
color, texture,
Are the nipples inverted,
Is discharge produced,
are nodules immobile,
is her quality of life reduced?
Take a moment… to be silent
With differentials and questions and familial history pooling in the mind,
For you must make space in this stillness of time,
To deliver a news that may shift the course of this rhyme
Take a moment…to reimagine,
That this couldn’t be you,
That you couldn’t be the one
To look in her eyes and deliver the troubling news,
It was the life you wanted,
The only specialty you knew,
But over the course of your training,
The weight of this burden grew,
Take a moment…to revisit
Those feelings that once were,
Filled with such promise,
That now feel so obscure,
Take a moment…to gather
Your thoughts,
your desires to serve in this space,
To counsel, to teach, to empower, and to share a thoughtful embrace,
To right the wrongs of centuries-old medical practice
With dignity, humility, and grace
You approached the field,
With only the thoughts of positive outcomes,
But failed to consider…when there wasn’t one,
Your story did not capture the woman who fell ill,
Or when the fetus had been delivered,
Cold, pulseless, and still
Take a moment…to process
How you revered in maintaining the health of the womb,
But after seven days on the service,
This vessel of life,
Evolves into a hollow, pear-shaped tomb,
Take a moment….to reconsider,
What life would be if you made more room,
To till the soil of your garden,
And allow for the seeds of destiny to bloom,
Take a moment…to look
Into the mirror and see what you’ve become,
Because there in that reflection,
There is a slight resemblance of someone,
Fragments of the old, but glimpses of the new,
Moments that reflect past passions,
but notes of what they had morphed into,
This desire to serve extended farther than that of the woman’s womb,
And in this infinite Eden of possibility,
My brainchild found room
Chapter II: Urology
Take a moment…to reset
To look at this rotation anew,
Because what you had been searching for,
had somehow found you,
It began with a knock on the door,
And a sheepish reply “You may enter”
Unconsciously I shift my attention to the woman,
But she is not who sits at the center
Take a moment…to view,
The air of defeat in the slouch of his posture,
Take a moment ….to recognize his courage to seek a doctor,
He peers up at you,
An emptiness in his gaze,
His wife quickly rushes over to hold his hand,
To somewhat mask the depth of his dismay
He tells me of their journey,
And how they’ve tried for years and years,
Until they sought the help of medical professionals,
Who would somehow ease their burgeoning fears,
He spoke of her strength,
Navigating conversations about her ability to conceive,
He spoke of her courage,
To defend and protect her family without reprieve,
Take a moment…to notice
The pain that continues to resurface,
And all that they had been through,
The waning support of their loved ones,
The constant judgement and ridicule,
Yet she sought answers,
she completed all the tests,
But when they all came back normal,
She entrusted him to do the rest,
Take a moment… to breathe
Take a moment…to seize…this moment that is before you
Take a moment… to see,
beyond the gown, the drape, or the anatomy
Take a moment… to listen to the history,
To the crackles in his speech, to his hesitation,
To the hum in his pause, to his tone’s vibration,
Take a moment… to view
What it is that stands in front of you
As his hand is carefully positioned atop his head,
And the gown is respectfully placed,
while ribbons gently touch the side of the bed,
and the slight embarrassed flush of his face
Take a moment…to inspect
the meatus and penile shaft,
Testicle, epididymis, spermatic cord,
Give yourself this moment to perfect your craft,
Are the testes symmetric,
Is discharge produced,
Are prostate nodules immobile,
Is his quality of life reduced?
Take a moment…to reimagine,
That this could be you,
That you would someday be the one
To look into his eyes and deliver the hopeful news,
It was the life you wanted,
Combining the admiration of a specialty you once knew,
Yet a new seed was planted,
With a flourishing destiny coming true.
====================================================================
Artist Statement:
This piece is dedicated to my grandmother, Claudette Cox-Brown, who exposed me to the intricacies and
delicacy of reproductive health. She served as a nurse midwife in Jamaica, England, and New York and shared with me so many
precious narratives of femininity, obstetric care, and the hardships of navigating pregnancy whether wanted or unwanted in
years past. Over time, the initial intrigue of her stories sparked an interest to pursue a similar path, and it followed me for a large
portion of my life. It paved the way for research opportunities in college focused on breast cancer, a medical mission’s trip to
Durban, South Africa focusing on the obstetric care of mothers and babies affected by HIV, my first career as a medical assistant
at an OB/Gyn office in Washington DC, and even the acceptance of a medical fellowship whilst in medical school, and for that I
am truly grateful.
However, this dream of mine to be an OB/Gyn never included the emergencies that happen in the delivery room. And
when things go awry, it happens fast. In my many experiences, I had always seen the outcome of healthy mother and healthy
baby, but never considered the possibility of losing either. My time in the longitudinal clerkship exposed areas of my journey that
I seemingly avoided, or hadn’t been privy to, and placed me in an emotional headspace I couldn’t escape. The beloved field that
had my heart for so long, had cemented wounds that had me question what the next step would be. In this poem, I address
some of those hardships, but also this love that I have for reproductive medicine transforming into something more, something
that created a space for old passions, but hopeful futures.
Urology has been that great awakening for me, not that I had slept through the life of undergraduate medical
education, but just an opportunity to see things both old and new with renewed purpose. Traits and behaviors that I had
perfected in my pursuit of being an obstetrician, have crafted my mindset about practicing urogynecology. I feel hopeful that my
interests in gynecologic procedures that focus on health after childbirth such as pelvic floor instability and urinary incontinence,
along with surgeries with the intent to tackle conversations that have are attached to social stigma such as female genital
mutilation and transgender medicine, can be cultivated in this field.
This poem takes you on that journey with me, the journey of facing those emotional hardships with the patient, and
within myself. Take a moment was written as my reminder to find some time, even just for a brief moment to be in that moment.
It is a mantra I use to escape my racing thoughts, to reconnect with patients, to observe, to reflect, and be mindful of the here
and now and sacredness of the space that my medical journey has afforded me. Take a moment though dedicated to my
grandma is a thank you to each obstetrician/gynecologist, midwife, nurse, charge staff, medical assistant, phlebotomist, practice
manager, and sanitation engineer that inspired and prepared me to seek and gain knowledge about every aspect of feminine
health. It is also a commitment to each urologist/urogynecologist, resident, and therapist who have accepted, mentored, and
exhibited patience and support as I worked to figure out the journey that lies ahead.

Shelby Wildish, Class of 2023
Character Description: Medical Student. Female. Late 20s. Eager to learn medicine, self-critical about self-expectations, general baseline tiredness. Wearing hospital issued scrubs, white coat, old worn-out sneakers....

Shelby Wildish, Class of 2023
Character Description: Medical Student. Female. Late 20s. Eager to learn medicine, self-critical about self-expectations, general baseline tiredness. Wearing hospital issued scrubs, white coat, old worn-out sneakers.
Scene: In Medical Student’s apartment living room. There is a big, colorful, soft chair with armrests in the middle of the room. Beside chair there is a standing full-length mirror. In walking distance from chair is a table, with a lamp, a cell phone, and a laptop computer. There is a rug on the floor and a small footrest.
====================================================================
[Enter Medical Student – she walks towards a chair, stops, turns to face mirror. She looks exhausted.]
MEDICAL STUDENT: You did it. You’ve made it to the end of another busy day. (Moves to sit down in chair, pauses to look down at feet) Damn, my feet hurt. I don’t know how Dr. Barterman does this all day. Walking up and down those long emergency room hallways, never getting a chance to sit down. It’s her shoes, has to be. She has some of those fancy clogs I’ve seen other docs wearing. I need to get a pair. Well, one day…(looks at old sneakers, then up at audience, shrugs)…when I can afford it.
Time to reply to the messages that came while on shift. I bet it’s the college roommate group chat blowing up about the recent girl’s Facetime chat. Another hangout without me; more group memories made without me. I find it interesting how quickly during quarantine it became the “norm” for social interactions to be almost entirely through computer or phone screens. Just shows human adaptability I guess… (Sits quietly, scrolling on phone, to self) I don’t even know what the update is about Amanda’s baby or Susan’s postponed wedding plans. I really need to call them – add that to the long To Do list.
(Looking at phone, slowly smiling then laughing aloud) I can’t believe they remembered that story! That was so long ago.
(Directed to audience) So, once I was dared to jump in frog fountain and then slipped while on the wall and fell face first into the water. (laugh, looking back to phone, nostalgic) we were all such idiots in undergrad. Such fun, but such idiots. I wonder what brought that up in the chat? (directed to audience) It feels good not to be forgotten. I remember this one time that Amanda, Susan, and I snuck into my brother’s house and stole his car during a snowstorm. Us three freshman girls, just trying to do some car drifting in the supermarket parking lot. I definitely need to remind them about it. (start typing on phone, to self) Too funny. (phone dings with notifications, medical student sits quietly, smiling and typing replies to the group chat.)
(Smiling, student puts phone down, looks off into the distance, demeanor changes to one of concern. Look around room, pick up phone and begin typing)
Guys, did you hear about those mass graves for unclaimed patients on an island near New York City?
(sits quietly)
(Irritated, speaking to audience) How can I be laughing when such things are going on in the world? I should be reminding my friends about the situation at hand. Bringing the conversation back to the patients, back to the families, back to the healthcare workers and back to COVID-19. (stand up, pacing and talking to self) Remember your reality. Remember the world’s reality. You wake up each day, and are reminded through new articles, research journals, social media posts, videos, and patient stories of the one sole focus – COVID. Don’t forget it has caused schools to close, businesses to shut down, economies to crash and nations to close their borders. It has caused millions to become unemployed, thousands to become overworked and all to become fearful. It has killed. It is killing. And it will continue to kill.
How dare you laugh? How dare you forget momentarily. (phone dings, student walks back over to the chair, glances at it, reads it, places it face down on armrest of chair, without replying.)
And you, you underestimated this virus’s capability, initially nonchalantly saying {in a mocking voice} “Oh, it’s just another influenza-like infection.” You felt a need to have a reassuring answer for concerned family members. When really, what you should have just said: “what do I know, I’m not even finished my second year of medical school.”
You incorrectly, and almost arrogantly, claiming it only affects the elderly and immunocompromised. Have you temporarily forgotten that you have three grandparents? Think of Nana, of Papa, of Grandma. This virus could take them from you. You are guilty of blissful ignorance. How lucky are you to be so far disconnected from any serious, immediate personal consequences that you have the luxury of having moments where you forget about everything, all things COVID-related. You’re lucky. Your family has been safe. Many families can not say that.
(walk slowly back to the chair, sit-down, pick-up phone and begins speaking while typing) The first patient this morning was a pleasant young guy, maybe 30. (To audience) Not that bad looking either. (back to phone) When we saw him, he was making jokes, laughing, even flirting with nurse Kelly… But you could tell he was having a really hard breathing. (To audience) His face was so pale. (back to phone) We got his oxygen levels. It was 86%. Dr. Barterman thought it was COVID and admitted him to hospital. That’s bad news.
(put phone down, stand up, start walking over to the table, stop, to audience.) At the end of the shift, we heard he wasn’t doing well. They found pneumonia in both lungs. He would probably need to be put on the ventilator. And the crazy thing, he doesn’t have any chronic medical problems. He runs marathons. He doesn’t do drugs, doesn’t smoke. He hangs out with his friends, has a dog. And before the quarantine, loved exploring the city. He is a healthy guy. Well, was a healthy guy.
Was a healthy guy.
(continue walking to table, pick up computer. Walk back to chair, sit down with closed laptop on lap.)
I can picture him, before all this COVID stuff, with a group of friends at a brewery. Joking around, laughing. Maybe even having one of those moments when you laugh so hard that you almost fall off your chair in joyful pain. I bet he is the type of guy that looks for the good in the moment. I bet he would tell you not to beat yourself up about reminiscing, almost as if encouraging you the laugh. You feel the sad, the guilt, the hard times, he would want you to feel the good too.
Isn’t that human nature? To feel. Emotions protect against apathetic eyes. Apathy has no past to base experience on. From feeling nothing for nothing, is no life at all.
(pause, look off in the distance for a while. Then re-center, and open laptop, click on a few buttons, slowly read out loud as if reading from phone) The FDA has approved the COVID-19 Pfizer vaccination.
Could this be it? A light at the end of the tunnel. A chance to get some element of normalcy back in life.
(stand up, beginning dialing on the phone, lift phone to ear, pace around) I have to get it. I need to get it for my family, for my patients. I need to get it so I always remember. Remember what COVID has done… what COVID is doing.
Hello, Dr. Barterman. Hi. It’s me, Savannah… Yes, I just saw the news article… I know! … Yes, it’s all so exciting! … It’s what we were hoping for… I can’t wait for when I can get it. Can you help me register? … Great, thanks … Of course I remember him… he what? … when? … Thank you for telling me.
He was healthy… was.
====================================================================
**This piece was a finalist for the inaugural Stethoscope Stage production
HuMed is a medical humanities and creative non-fiction online journal featuring thematic writing, along with other forms of humanities-based contributions from students, faculty, and staff.
The Dallas Morning News
The Dallas Morning News
Insight Into Diversity Magazine
KERA News