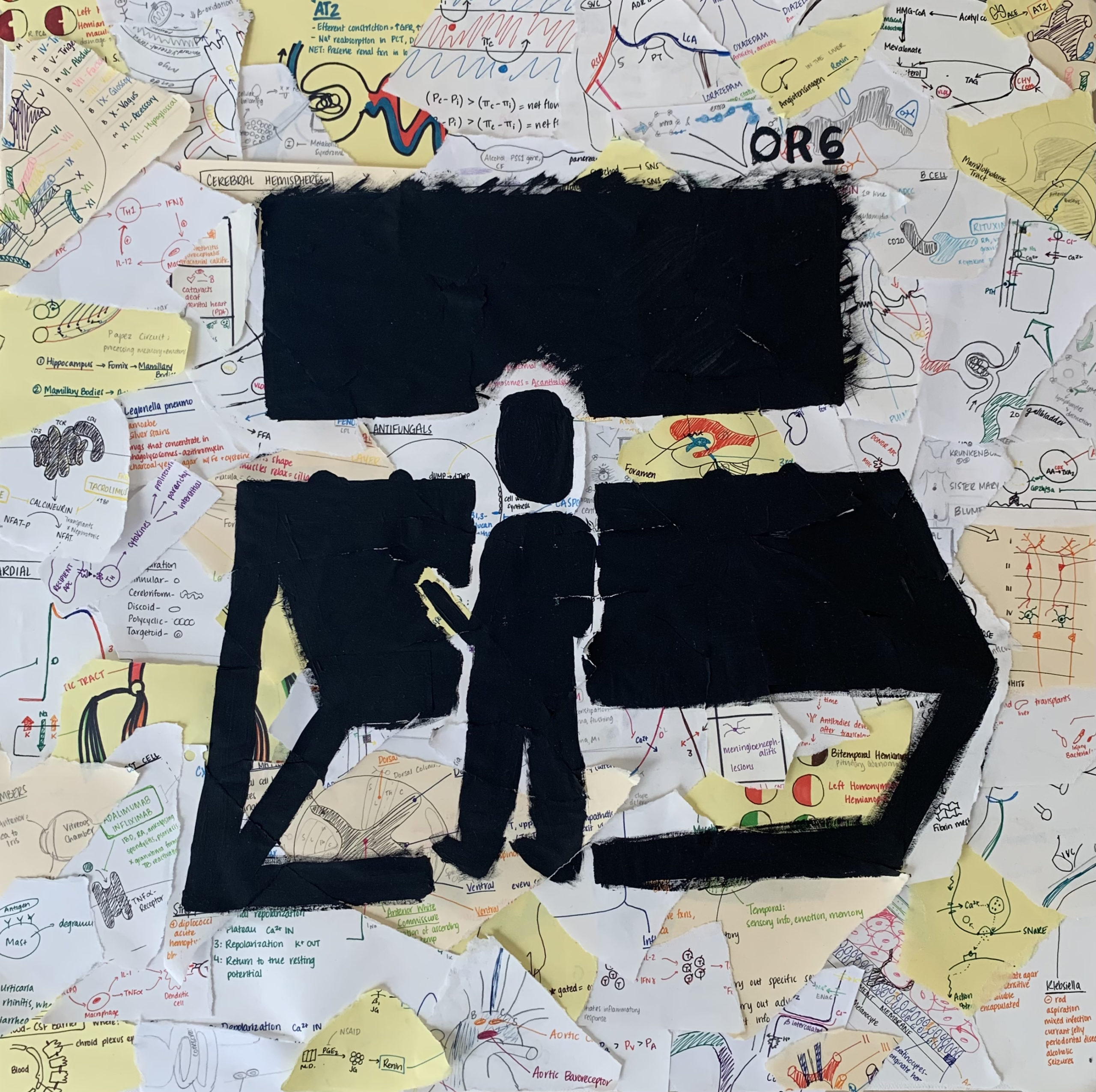
Character Description
Kavneet: A naïve 3rd year medical student working a shift in a rural Emergency Department at the time of yet another COVID surge. Must work shifts for 28 out of 31 days this month. Tired, but ready to work and take on a challenge. Always hopes for the best and tries the see the good in a bad situation.
Scene: It is month 8 of 10 of my Emergency Medicine rotation and delta variant reared its ugly head.
====================================================================
[Cruising down the highway at the crack of dawn with the window rolled down, I let the cool, crisp air wake me up. The radio is screaming on repeat: “The death toll from COVID-19 is increasing day by day… Delta variant seems to have world leaders worried of yet another spike in cases”. As I pull into the parking lot, two deer cross in front of me near the entrance of the hospital. You don’t get that in the city.]
Hour 0
KAVNEET: “How is this shit still going on?” I grumble to myself as I walk over to greet my attending in the breakroom. I notice the tracker board with the list of current patients… just when I thought I was going to have a ‘Q word’ day.
“Q word” means “quiet”, but you don’t dare say that word in the ED unless you want all your staff cursing you out an hour later while being knee deep in patients that decided to take a trip to your emergency resort.
I overhear the overnight attending pass off a patient to my attending physician, who in disbelief remarked “This was the same patient I had on shift two days ago.” The patient is COVID positive and is currently waiting to be transferred to another facility for more intensive care, but no hospital nearby is accepting patients.
They have now been in isolation for more than 72 hours. Imagine a 6-foot by 6-foot room with white walls and no windows. No human contact outside of nurses coming in to give you meds or adjusting ventilator settings. Sedated. Looking more machine than human. Listening to the music of the vital monitor beeping similarly to a ticking clock, amid chaos happening in the room to the left and to the right of you. Lifeless.
It is quite literally the closest thing to solitary confinement without being imprisoned.
My trance breaks as we rush through the remainder of the patient list. I notice there are others waiting more than 40 hours needing to be admitted to the second floor for inpatient care.
Here’s the thing that the public tends to forget- there are still a portion admitted patients in need of critical care, who do not have COVID. This could be your grandfather having his first heart attack, your significant other that just got into a car crash or is having a miscarriage, or your child that is about to slip into a diabetic coma.
And the fact of the matter is that there may not be a place to put them or stabilize them. Even if we can, they are still left waiting for another hospital to “accept” them to get the care that they need.
Why does someone need to be interviewed to see if they are sick enough to be treated? How does that make sense?
Hour 2
KAVNEET: More patients are checking in. COVID patients get priority, especially if they have a below desired oxygen level. In other words, “priority” means you can be put in a room with an actual door that closes. What do we do when those rooms run out you ask? I pray to God. You pray to whatever Higher Power you believe in or just hope for some good vibes. “We have NO rooms open for COVID patients!” I hear the charge nurse scream as if it was not obvious. Though by the look in her eyes, more a scream of frustration than one to state facts. Let those prayers begin. We now have no option but to fill in these makeshift “rooms” with possible COVID patients. Picture a room divided into smaller sections by a shower curtain instead of an actual door. I try to justify it to myself as, “well, it’s not like there is any other place we can put them, and we can’t just stop seeing patients.”
Hour 3
KAVNEET: I do the best I can to help my attending and the staff see patients. At one point, I go to the front to help triage patients, some of whom had now been waiting for at least an hour. Our triage room is quite literally the size of a closet, so you can imagine how this was about to go.
With my head held high, a N95, surgical mask, and face shield, I march into the lobby and scream the first patient’s name to bring them into our broom closet. Yes, scream…it is that chaotic. I ask what brought them to our ED today. Cough, fever, shortness of breath? What a shocker.
“Have you been vaccinated?” I question with skepticism. No? Surprise, surprise. I proceed to get the vitals. Blood pressure 142/94… eh, won’t kill you, temperature 99.8… low-grade fever, heart rate 104… tachycardic, oxygen saturation 92… mildly hypoxic. Yep, this is to be expected. Ok now to swab for COVID.
Like clockwork, now onto the next one.
Hour 3.5
KAVNEET: We officially maxed out on the makeshift rooms, but we still have a lobby full of unseen patients. “What can we do? I understand we don’t have any space to put them, but we can’t turn them away,” my attending physician shouts through his N95 to the charge nurse as he rushes to check on a critical patient that just came in with low oxygen saturation. “PAGE RRT STAT”.
34-year-old female, with oxygen saturation in the 50s.
As my attending and others work to assess the gravity of the situation, the rest of us manage to add two gurneys and a chair… three extra spaces in the hallway of our small boondocks ED. If a code blue walks in through the door right now, we would literally be doing it in the ambulance bay outside of the hospital. Totally code compliant.
I rush back to the critical patient that was brought in. Everything and everyone moved like an assembly line. Prepare the meds, sedate, paralyze, intubate, get out. I open her chart and glance through it. She is a healthy young woman without any health conditions. She has had COVID-like symptoms for 2 days and began to develop shortness of breath overnight. So why is she this bad? Something is not adding up…Vaccination status? Unvaccinated.
As we exit the room, the front door almost knocks me down as the medical director of the Emergency Department darts in through the door. Before I can process, monitors start going off. BEEP BEEP BEEP! The patient that we just intubated… a bunch of staff rush in and one of the nurses’ pages RRT again. Oxygen saturation is 70. I stand outside the room as I see the panic in everyone’s eyes. There’s simply no time for this right now.
My attention diverts behind me as I overhear the charge nurse and medical director calling hospitals from DFW to College Station to find beds so they can move our current patients out to add new ones to the trenches. The medical director even made a personal call to the CMO of the hospital system. Little did I know that in the last several hours, we were still getting calls from the transfer center to accept patients from Kansas.
Hello? What happened to the entire state of Oklahoma?
Hours 4.5 to 9
KAVNEET: We come up with a plan to open a currently unused space on the second floor to put some non-COVID, lower acuity patients. One of the nurses told me this is the first time since the pandemic began 1.5 years ago this was being done. And for the first time since beginning my shift, I force myself to find a moment to stop and take in what is going on around me.
Do you think if an unvaccinated person saw face to face what it looks like to have more than a “COVID cold”, they would change their mind about getting vaccinated?
I often think about that young lady on the vent. If she made it off, her life will never be the same.
On a systemic note, I’m still trying to grasp how we got here? I see nurses, techs, RTs, pharmacists, radiology techs, and physicians running around the hospital trying to do the best they can, trying to solve problems that were created by this system, trying to juggle tasks out of the scope of their practice on top of their normal duties because there is no one else there to do it. I am appreciative of how hard each team member worked in our small ED that day. They are the true embodiment of perseverance and fight.
On top of dealing with a public health crisis, the unfortunate reality of working in a small ED such as this one is that patients are at risk of dying, simply because they cannot get to another facility for more intensive care. Bigger city hospitals will not accept more patients because they are also being bombarded with COVID, and statistics show that most of these patients are also unvaccinated. Even then, at least the bigger hospitals are equipped with resources and specialists to handle the surplus. To put it into perspective how smaller, boondocks EDs are affected, if you are unfortunate enough to come on the wrong day, your options are to talk to someone through an iPad or get transferred to another facility that has someone physically there to take over your care. Often, it’s the latter and we are 40 minutes from the nearest big city hospital.
If being vaccinated means less stories like what you just heard, less burnout for the people who are tirelessly and endlessly taking care of you and your loved ones, less loss of the ones you hold close to you and heck, maybe even you yourself. The question I then pose to you is: If you do not have a legitimate medical reason to not get vaccinated, what is the hesitation to get the vaccine? Whether you are pro-vax or vaccine hesitant, we can all agree that we are mentally and physically tired of this and want life to go back to “what it used to be”.
====================================================================
**This piece was a finalist for the inaugural production of Stethoscope Stage